The next challenge is figuring out what your BP actually is. With this remark I invite mockery, but I put some effort into getting good readings and found the process discouraging. I have to sit for five minutes relaxed with nobody speaking to me, and my device is probably not on the magic list???
Honest question, what is the value in that if that is not my daily life?
Is it really THAT much effort, considering how fundamentally important blood pressure is to your health? Just invest in a decent quality Omron BP monitor and sit for 5 minutes, for heavens sake. You can even check it at 1 or 2 min, and if you’re at goal, no need to wait the full 5.
Just took my BP at home 105/55 SBP/DBP and 80 bpm. Should I be worried about the low DBP of 55? The only BP med I take is 20 mg Telmisartan.
This is quite wild as a year ago it was 135/80. What happened??? The high number is from the Dr. office and the low numbers from a home cuff. Not sure what to believe.
I would like to kow too as I have generally have low BP, last night 93/54and this morning 106/55.
First, you can’t just take one measurement, preferably take three and average them. There may also be some imprecision in your device or technique of taking the measurement. Officially, low BP is SBP below 90, DBP below 60, so 55 is a little low.
However, I would be more concerned about pulse pressure, as your PP is 50, which is starting to be higher than desired, and might be indicative of suboptimal function.
That’s the number I’d watch in your case, assuming your measurements are legit and persistently at or above 50.
How do you determine PP?
PP is calculated by taking SBP - DBP.
If your blood pressure is 140/70, that means your pulse pressure is 70 (difference between the two numbers). Ideally, you want pulse pressure at about 40
Its unclear how much the blood pressure went down in the treatment group:
Paywalled Research Paper:
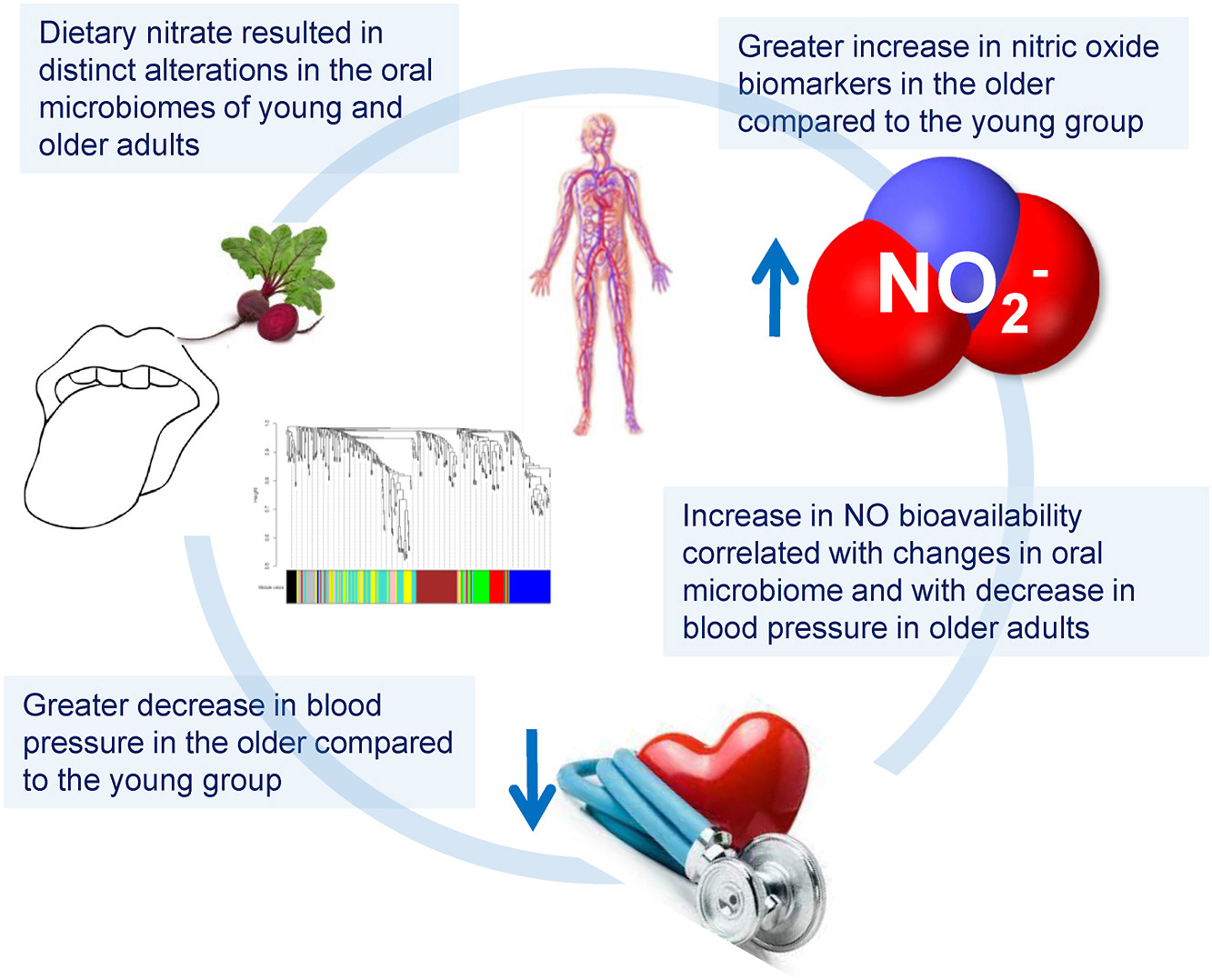
Ageing modifies the oral microbiome, nitric oxide bioavailability and vascular responses to dietary nitrate supplementation .
Free Radical Biology and Medicine , 2025; 238: 682
How does “secretly” apply to this? Has clickbait phrasing infected science reporting? Confused.
Clickbait phrasing secretly infected science reporting some years ago.
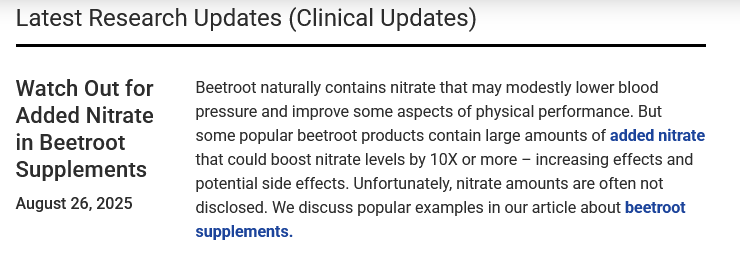
A recent report on ConsumerLabs indicates that many beetroot supplements have been “supplemented” with extremely high levels of nitrate. Which can drop BP way too low.
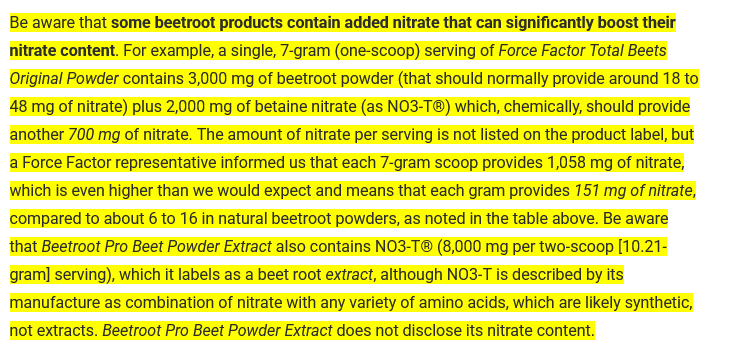
New study: The data showing net benefit for lower targets is compelling, but you can’t ignore the real risk of harm, especially for older adults.
Benefit–harm trade-offs of intensive blood pressure control versus standard blood pressure control on cardiovascular and renal outcomes: an individual participant data analysis of randomised controlled trials
he initial dataset included 80 676 participants, of whom 80 220 were included in our analyses (intensive blood pressure control group n=40 503; standard blood pressure control group n=39 717). The median age was 64·0 years (IQR 59·0–70·0), 39 043 (48·7%) participants were male, and 41 177 (51·3%) were female. Most participants were Asian (66 290 [82·6%]) or White (8097 [10·1%]). During a median follow-up of 3·2 years (IQR 3·0–3·5), the composite cardiovascular disease outcome occurred in 2158 (5·3%) participants in the intensive blood pressure control group and 2811 (7·1%) participants in the standard blood pressure control group (hazard ratio 0·76, 95% credible interval [CrI] 0·72–0·81; p<0·0001). Compared with standard blood pressure control, intensive blood pressure control was associated with a 1·73% absolute risk reduction (95% CrI 1·65–1·81) in cardiovascular disease (number needed to treat 58 [95% CrI 55–61]) and a 1·82% absolute risk increase (95% CrI 1·63–2·01) for adverse events of interest (number needed to harm 55 [95% CrI 49–61]). Overall, intensive blood pressure control showed a favourable benefit–harm profile, with a net benefit of 1·14 (95% CrI 1·03–1·25), using adjudicated weighting. The net benefit remained positive when considering kidney-related adverse events (1·13 [95% CrI 1·01–1·24]).
Interpretation
Compared with standard blood pressure control, intensive blood pressure control provides a net benefit between the reduction in cardiovascular events and the increase in adverse events, including renal events.
Paywalled paper:
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(25)01391-1/abstract
I’m taking 80 tel and 5 amlod, which gives me a typical morning reading of 120/77/52. The SBP will vary throughout the day, often by 10 or 20 points, which AI says is normal. I wanted to change the amlodipine for nebivolol, but the latter can’t be prescribed for an HR of less than 60.
I’ve been taking febuxostat, which helps with both the swelling caused by gout and the swelling caused by amlodipine. This strategy has been working well. But now with the tariffs, my source of febuxostat has been cut off, and my nephrologist, who is a little uptight, will freak out when she learns that I have been self-prescribing. I will be labeled non-compliant.
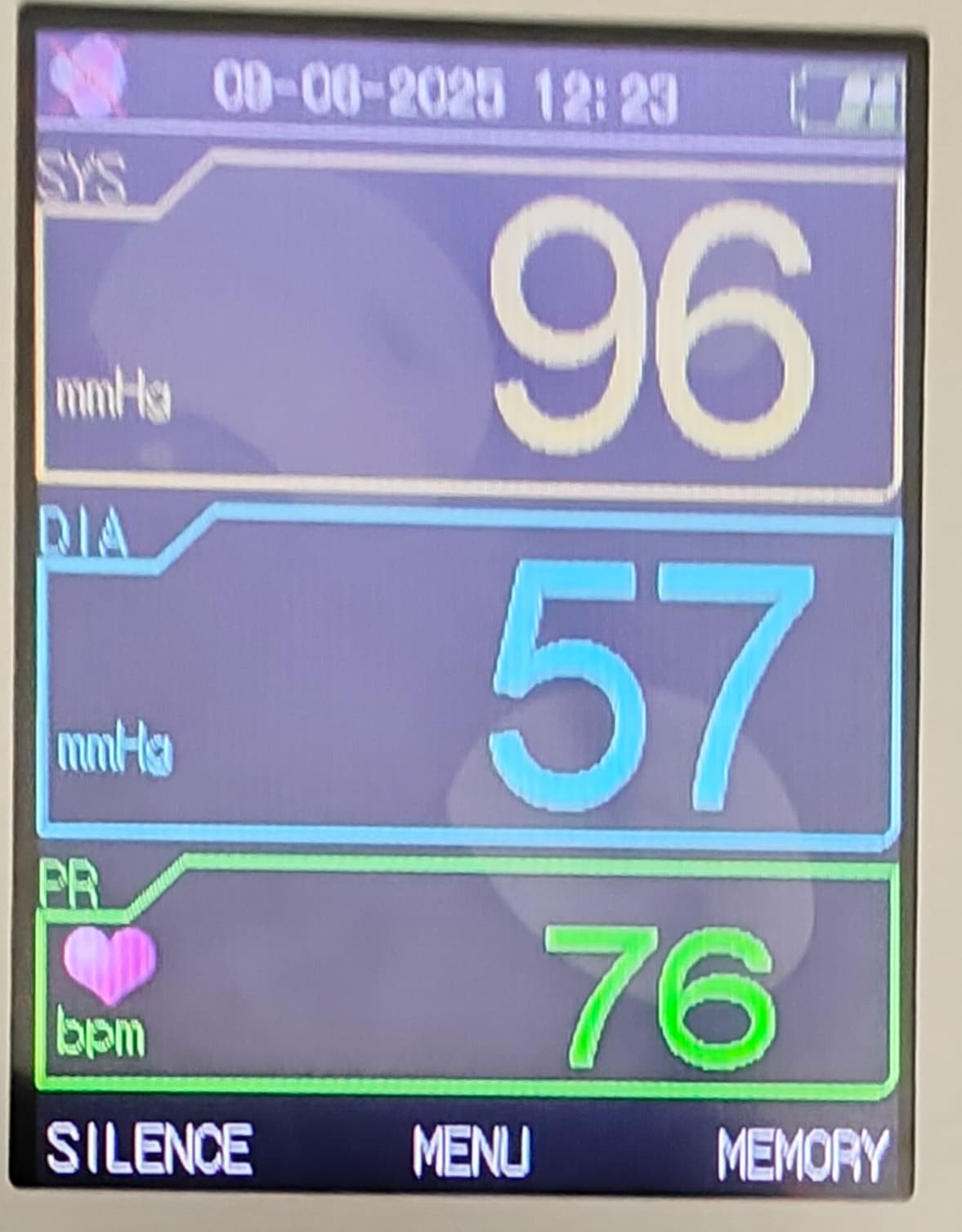
I really don’t understand what’s going on. My blood pressure is continuing to drop. I took this reading at noon today when SBP is supposed to be the highest. I didn’t even take my Telmisartan. PP is 39 and RHR is improving. Any thoughts?
Before taking Telmisartan, my SBP was typically in the 125-145 range. The only BP lowering supplement I am taking is citrulline after dinner.
A drop of 20–40 mmHg in systolic blood pressure can happen for a variety of reasons, some benign and some clinically important. It’s often context-dependent (e.g., position changes, illness, medications). Here are the most common categories:
1. Physiologic / Situational
- Orthostatic hypotension: Standing up from sitting/lying can transiently lower systolic pressure by 20–30 points, especially if dehydrated, on certain medications, or in older adults.
- Post-exercise: After strenuous exercise, vasodilation in muscles can briefly reduce systolic BP.
- Postprandial hypotension: In older adults, blood pools in abdominal vessels after eating, lowering pressure.
2. Volume Depletion
- Mild to moderate dehydration: From not drinking enough fluids, sweating, or illness with vomiting/diarrhea.
- Blood loss (non-massive): A moderate GI bleed, heavy menstrual bleeding, or slow internal bleeding may drop systolic pressure in the 20–40 range before shock develops.
3. Cardiovascular Causes
- Arrhythmias: Atrial fibrillation with rapid ventricular response, premature beats, or bradyarrhythmias may lower systolic pressure intermittently.
- Heart failure exacerbation: Reduced stroke volume can cause noticeable BP drops.
- Medications affecting preload/afterload: Nitrates, diuretics, or strong antihypertensives can all lead to a 20–40 point reduction.
4. Vasodilation / Autonomic Causes
- Medications: Beta blockers, ACE inhibitors, calcium channel blockers, alpha blockers, or vasodilators can lower systolic BP in this range.
- Alcohol or sedatives: Can cause vasodilation and lower pressure.
- Autonomic dysfunction (neuropathy): Seen in diabetes, Parkinson’s disease, or after certain neurological injuries.
5. Acute Illness
- Early infection / sepsis: Sometimes the first clue is a modest drop in pressure before shock develops.
- Allergic reactions (mild–moderate anaphylaxis): Can cause systolic pressure drops in this range if not severe.
- Adrenal insufficiency: In Addison’s disease, BP may be persistently low or fluctuate downward with stress.
 When it matters
When it matters
- Transient drops (e.g., standing, after meals) are often benign but may increase fall risk.
- Persistent or symptomatic drops (lightheadedness, fainting, chest pain, confusion, cold skin) can indicate a serious underlying problem and should be evaluated.
- In medical definitions, a ≥20 mmHg systolic fall upon standing is one criterion for orthostatic hypotension.