@John_Hemming
If I had a blood test every week, I wouldn’t have any veins left.
Luckily my protocol appears to speed up wound healing so the arm I normally use normally has the prevoius week’s wound disappear before the next puncture. I have just taken a photo and will attach it t this post. My last venepuncture was on Wednesday and today is Sunday.
Sorry for the late reply. That’s a little high ratio but it’s fine.
Yes I personally would keep the ratio of EPA/DHA somewhere between 1:1 and 2:1.
Attia weighs in on Omega-3 and AFib.
Looking at his take from that article
So what’s my take? An association between supplemental n3FA and increased risk of AFib seems likely to exist, but perhaps only for those already at significant risk for cardiovascular events. Current research using existing data is further interrogating the question of n3FA supplementation and associated risk of AFib and may help shed light on how such an association might depend on prior CVD risk factors. The Global Organization for EPA and DHA is currently conducting its own meta-analysis covering a large number of studies, and the Fatty Acids and Outcomes Research Consortium, which has collected massive volumes of lipid data from study populations over many years, is looking now at AFib endpoints among its datasets. Pending further insight, all patients who are advised to take supplemental or prescription n3FA products should also be advised of the potential risks, and caution is warranted particularly for those with a predisposition to AFib. Given the existing evidence that n3FA supplementation may alternatively reduce CVD-associated risk, I weigh the benefits with the risk for each patient, and individual characteristics like heart rate, HRV, TG, and CVD history are important considerations to assess whether n3FA supplementation provides more harm or benefit.
There is a probably a threshold with Omega 3 when the level of supplementation causes some issues.
I did experiment with Omega 3 a couple of years ago and found that when I stopped taking supplementary capsules twice a week I noticed a deterioration. I now take a capsule a day 3g of fish oil 1.3g EPA 0.9g DHA. There is no massively complex calculation behind this. I don’t think there is any doubt that this helps with the formation of better quality membranes. Where the AFib risk is in terms of dosage I don’t know.
I have got my resting heart rate back down below 50 mainly through not drinking as much as I was and am otherwise doing quite well in terms of a range of tests. Hence I intend to stick with one of these capsules a day.
Fuhrman recommends Omega-3 index above 6. Most people 250 mg EPA+DHA should work. Too much not good either (bleeding risk, AFIB?). The longer time the better.
It takes 3 months for blood cells to change or something, so when intake can change the Omega-3 index result.
I don’t think people should look at only short-term gains. Things are looking exponential and compounding…?
You are taking Vetology algae omega-3, which contains 300mg EPA and 500mg DHA. Would you reduce this to just one capsule per day?
Yes but you can measure Omega-3 index after awhile to see if you need more to get to the index level you want (depends on genetics for absorption, some might need more to get above 6, or whatever number someone picks).
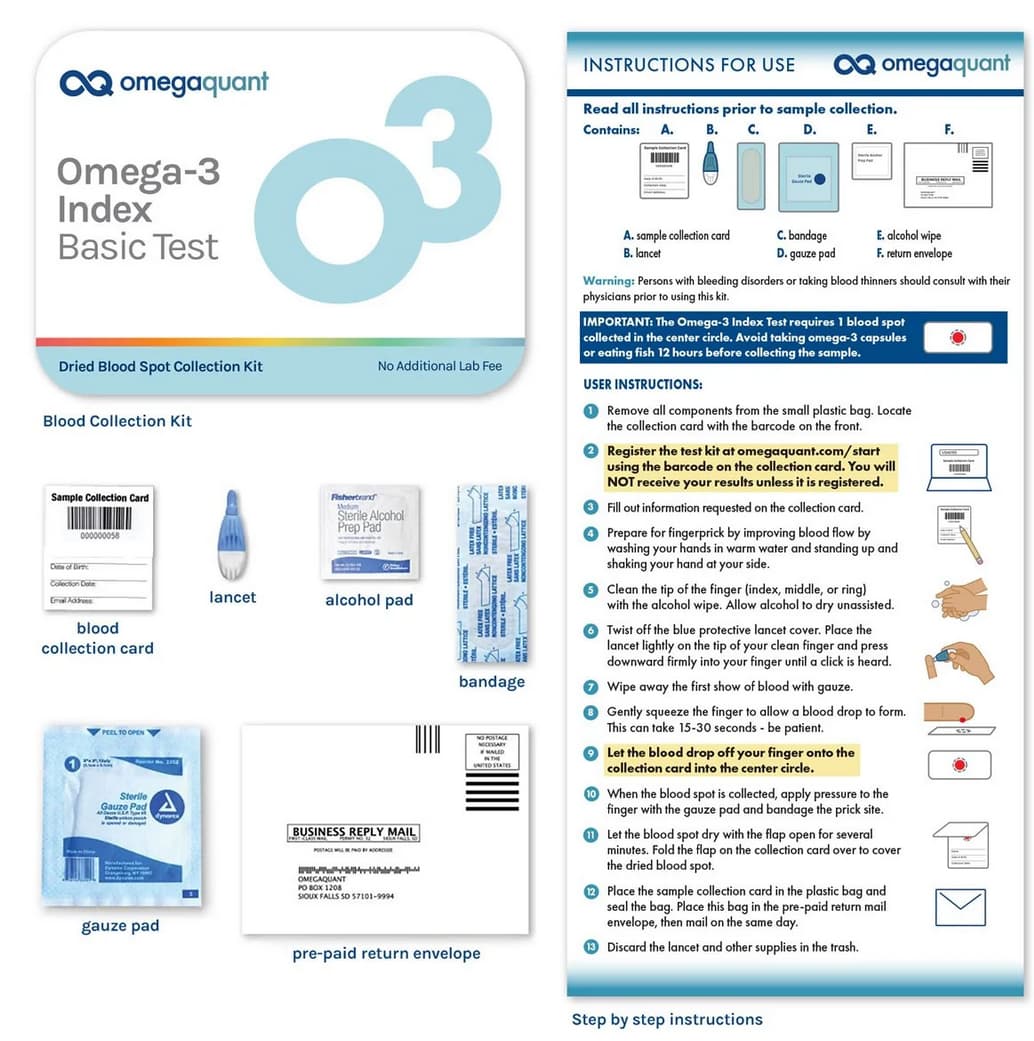
Did you find a way to measure this? I haven’t found any labs in Europe offering such a service.
The test from OmegaQuant seems professional:
Can get it from different places (this is one it seems).
I just take a single omega 3 pill daily and eat 150-200 grams of walnuts each week. That should be enough to cover my omega 3 needs since I utterly despise the taste of fish.
You can test your Omega-3 index, that seems the best idea to determine whether you need more, or even if you are eating too much. I don’t know what the optimal percent is for sure.
Maybe or maybe not. The issue is your Omega 6:Omega 3 ratio. If you have have a less than 4:1 ratio, the enzyme, delta-6-desaturase (which Omega 6 and 3’s compete for) that converts omega 3’s in walnuts (alpha-linolenic acid) and other plant based foods into DHA/EPA isn’t sufficiently active. So formally checking an Omega 3 index is necessary to know. Direct supplementation of EPA/DHA is often necessary as vegans run ~3.5, vegetarians ~4%, and Standard American Diet ~4.5% - with goal being 8-12%.
Do we know anything about what impact being above 12% has? I saw a video from the OmegaQuant people, and they said something like there are not enough people with measured levels that high for studies to have incidentally included enough of them to be able to have much existing observational evidence about the consequences.
High doses risk atrial fibrillation, and excess stroke. I do mine with goal of 8-9% personally as there is a sweet spot, which is why one needs to measure.
I just received my Omega test this morning. I was surprised that my Omega 3 level was only 5.1%. I eat fish 2-3 times per week and take 1.25 grams of fish oil (EPA 750mg, DHA 285mg, DPA 50mg) a day. Going to up the fish oil to 2.5 grams and see what that does.
What “low” means
Most labs now use the Omega-3 Index (O3I) — the percentage of EPA + DHA in red-blood-cell membranes.
- < 4 % = clearly deficient (higher CVD and all-cause mortality risk)
- 4–8 % = intermediate
- 8–12 % = the “optimal” band seen in Japan, coastal Korea, and most RCTs showing benefit
How much does 500 mg/day move the needle?
Daily EPA + DHA dose Typical 4- to 5-month change in O3I Chance of hitting ≥ 8 % 300 mg ≈ +0.3 – 0.6 % Essentially 0 % 500 mg ≈ +0.5 – 1.0 % (large inter-individual spread) Rare unless you started at 7 % 600 mg Mean endpoint ≈ 6 % in an RCT 0 % of participants reached 8 % (GrassrootsHealth) 900 mg Mean endpoint 7.5 % ~25 % reached 8 % (GrassrootsHealth) 1 000 – 1 500 mg +2 – 5 % in 3–6 mo Often crosses 8 % if baseline > 4 % (PubMed Central) 2 000 mg Modelled to lift 5.4 % → 8 % in 20 wk Very likely for most adults (Mayo Clinic Proceedings) Key point: 500 mg/day is the minimum many guidelines cite for general health (Office of Dietary Supplements), but dose-response data show it usually nudges a truly low O3I upward only modestly. It is seldom enough to exit the high-risk < 4 % zone, let alone reach ≥ 8 %.
Why responses differ
Baseline status – the lower you start, the bigger (in absolute %) each gram produces.
Body size & adiposity – larger lipid pool dilutes incorporation.
Chemical form & timing
- Re-esterified triglyceride or phospholipid (krill/algal) > ethyl-ester on an empty stomach.
- Always take with a fat-containing meal; splitting BID slightly improves retention.
Dietary ω-6 load – high linoleic acid competes for the same membrane slots.
Genetics (FADS cluster) – “slow desaturators” need 15-30 % more intake to hit the same O3I.
Practical roadmap for an ovo-vegetarian who minimises calories
Step Rationale Calorie cost 1. Measure baseline O3I (finger-prick kits are <$50). Individual variation is huge; testing beats guessing. 0 kcal 2. Start at 1 000 mg EPA + DHA/day via algal oil (e.g., two 500 mg capsules). Likely to raise O3I by ~2 % in 3 mo; still only ~9 kcal. ≈ 9 kcal 3. Re-test after 12-16 weeks. Full RBC turnover is ~120 d. — 4. If still < 8 %, double to 2 g/day or cut dietary ω-6 (seed oils, commercial snacks). Dose–response and ω-6 reduction are synergistic. ≈ 18 kcal 5. Maintain vitamin E (mixed tocopherols 100–200 IU) & selenium 55 µg to protect the newly enriched membranes from peroxidation. Prevents paradoxical oxidative stress. negligible When 500 mg is enough
- You already sit in the 6–7 % band and just want maintenance.
- You eat ≥ 2 portions/week of oily fish (not applicable here).
- Your goal is minimal support for pregnancy (many obstetric bodies set 300–500 mg/d).
When you need much more
- Triglyceride lowering: Rx preparations use 2–4 g/d EPA ± DHA.
- Post-MI cardioprotection: AHA guideline is 1 g/d, often titrated higher if O3I < 8 %.
- Anti-inflammatory or neuropsychiatric protocols (e.g., depression with high CRP) routinely test 2–4 g/d.
Bottom line
A steady 500 mg/day of EPA + DHA will usually move a deficient Omega-3 Index upward, but only by about half a percentage point – rarely enough to leave the “low” category. For a robust, evidence-based correction, plan on 1–2 g/day for 3–4 months, then adjust based on a repeat blood test. The extra calories (≈ 9–18 kcal) are trivial compared with the cardiovascular and cognitive dividends of reaching ≥ 8 %.
What the evidence actually shows — and what it doesn’t
Red-cell Omega-3 Index (EPA + DHA % of total RBC fatty acids) Typical daily intake needed Effect on in-vivo lipid-peroxidation markers (MDA, F₂-isoprostanes, 4-HNE) Key data < 4 % ≤ 250 mg Highest baseline levels of MDA/F₂-Iso; correcting ω-3 deficiency lowers them. Large meta-analysis of 47 trials of ω-3 dosing < 1 g reduced MDA by −0.38 μmol/L vs control (ScienceDirect) 4 – 8 % 0.5 – 1 g Neutral to ↓ lipid-peroxidation; most RCTs report either no change or small decreases. Review of 20 human studies found zero increase in 4-HNE or TBARS at intakes ≤ 2 g/d (Wiley Online Library) 8 – 12 % (Japanese “coastal” range) 1 – 2 g Consistently lower MDA and urinary F₂-Iso; shift from 9-HNE (ω-6-derived) toward the milder 4-HHE (ω-3-derived). Mori et al. GC-MS F₂-Iso study (1.8 g/d, O3I ≈ 10 %) (Frontiers) 12 – 15 % 2 – 4 g Data sparse; most trials still show no rise provided vitamin E ≥ 10 IU per g fish-oil is present. Hypertensive-diabetic cohort on 4 g/d: F₂-Iso fell 22 % despite O3I ≈ 13 % (PMC) > 15 – 16 % > 4 g for months Isolated reports of mild uptick in MDA or conjugated dienes when antioxidants are low; also where bleeding and atrial-fib risk starts to climb. Review of high-dose CV trials notes safety concerns appearing at O3I > 16 % (research.rug.nl) Bottom line: No reproducible threshold exists inside the commonly targeted 8–12 % band at which ω-3 PUFA start driving oxidative damage. Most real-world signals of acrolein, 9-HNE or F₂-isoprostanes fall, not rise, as the Omega-3 Index climbs from deficient to optimal.
Why higher ω-3 does not automatically mean more 9-HNE or acrolein
Origin of the aldehydes matters.
9-/4-HNE and acrolein are largely downstream of ω-6 arachidonic or linoleic acid oxidation. Raising EPA/DHA lowers the ω-6 : ω-3 ratio and crowds AA out of membranes, so the very precursors of 9-HNE drop. (PubMed)Different aldehydes, different potency.
DHA peroxidation yields 4-hydroxy-2-hexenal (4-HHE), which is 3- to 10-fold less electrophilic than 4-HNE and can even activate the Nrf2 antioxidant program. (PMC)Antioxidant buffering.
Trials that did report a blip in peroxidation at very high ω-3 intakes used oils with < 2 IU vitamin E per g and subjects with low Se/α-tocopherol status. Adding 100–200 IU of mixed tocopherols or co-ingesting fruit/vegetable polyphenols abolished the rise. (Cambridge University Press & Assessment)Ex-vivo vs in-vivo confusion.
Yes, poorly stored fish oil oxidises readily and can generate acrolein—even at room temperature. (J-STAGE) That has little to do with the peroxide load inside your red-cell membranes, which are enzymatically protected and constantly repaired.
Practical guidance
Goal Target Omega-3 Index Daily EPA + DHA (re-esterified TG or algal) Antioxidant pairing Correct deficiency 8 % 1 g for 12 weeks, then re-test 100 IU mixed tocopherols + 55 µg Se Sustain optimal 8–12 % 0.8–1.5 g, or 2 oily-fish meals / wk Diet rich in carotenoids/polyphenols High-dose therapy (TG lowering, inflammation) 12–14 % 3–4 g under supervision ≥ 400 IU vitamin E/day & monitor MDA or F₂-Iso Do not exceed† ≈ 16 % > 5 g chronically benefits plateau; bleeding & AF risk edge upward †The European Food Safety Authority flags > 5 g/d long-chain ω-3 as the point where safety monitoring is prudent; this corresponds to an Omega-3 Index in the mid-to-high teens for most adults. (research.rug.nl)
Take-aways for someone worried about oxidative damage
- Stay in the 8–12 % “sweet spot.” It maximises cardiovascular and cognitive benefit while keeping oxidative markers flat or lower.
- Use fresh, N₂-sealed products. Smell the oil: a paint-like, fishy odour signals pre-formed aldehydes—you’re swallowing the oxidation instead of making it.
- Always feed the antioxidant network. The rule of thumb is ~10 IU of mixed tocopherols per gram of EPA + DHA plus selenium-dependent GPx cofactors.
- If you must push >3 g/day, measure both sides of the ledger. An at-home finger-prick Omega-3 Index kit plus urinary F₂-isoprostanes or plasma MDA every 3–6 months will tell you whether your antioxidant capacity is keeping up.
Summary
Current human data show no meaningful rise in acrolein, 9-HNE, 4-HNE, MDA, or F₂-isoprostanes until the Omega-3 Index approaches the mid-teens, a zone reached only with pharmacological fish-oil dosing and inadequate antioxidant cover. For everyday health optimisation, aim for 8–12 %, pair ω-3s with ample tocopherols-plus-polyphenols, and rancid-oil worries become a non-issue.
This seems to be low-quality BS that you copied-pasted from ChatGPT @AlexKChen. DHA supplementation is detrimental, meanwhile EPA supplementation might have cardiovascular benefits: Vitamin O (Omega 3) for athletes - #4 by adssx