I asked o3 for a longer transcript
Below is a “tidied-up” transcript—the video is still presented chronologically, but I’ve:
- removed repeated greetings, filler words (“um,” “you know,” etc.), long pauses, and on-screen music cues
- merged sentences for flow and fixed obvious grammar/punctuation errors
- kept timestamps at key transition points so you can still navigate back to the original video if needed
- lightly paraphrased a few phrases for clarity (technical terms are unchanged)
0:00 – 1:30 Welcome & Set-up
Good morning, afternoon, or evening—depending on where you are.
We’re starting an hour later than planned because I had to finish a Medicare-project meeting and had some last-minute studio glitches.
Today’s topic: how to measure cardiovascular inflammation, the real driver behind heart attacks and strokes. Most doctors still focus only on LDL cholesterol.
1:30 – 4:00 Why Cholesterol Isn’t the Whole Story
Yes, plaque contains a lot of cholesterol, but cholesterol isn’t the problem until you irritate the arterial intima (the single-cell lining of every artery). When that lining is “burned,” LDL sneaks through and starts an immune cascade.
4:00 – 6:30 Doctors Miss Pre-Diabetes & Insulin Resistance
Primary-care physicians routinely overlook insulin resistance, even though it causes most heart attacks, strokes, blindness, and kidney failure. That’s why I created webinars, online courses, and the book “Prevention Myths.”
6:30 – 9:30 Misconceptions & The Inflammatory Spiral
Myth: “A stress test will tell me if I’m going to have a heart attack.”
Reality: Stress tests detect ≥50 % arterial blockage, not soft plaque.
When the intima is damaged, oxidised LDL attracts monocytes → macrophages → foam cells. Cytokines thin the fibrous cap; rupture + clot = heart attack or stroke.
9:30 – 12:30 Markers Rise in Sequence
A typical progression: Oxidised LDL → high-sensitivity CRP → Myeloperoxidase (MPO) → LP-PLA₂ → high-sensitivity Troponin T.
12:30 – 18:55 The Five Tests I Order Most
- Oxidised LDL – difficult to obtain but useful if available.
- hs-CRP – good screening tool, but many false positives (e.g., after a flu shot).
- Micro-albumin/creatinine ratio – best window on intimal “leakiness.”
- LP-PLA₂ (Plaque-2) – enzyme released by activated macrophages.
-
MPO – enzyme from neutrophils; highly specific for arterial inflammation.
(IL-6 is informative but we don’t order it routinely.)
18:55 – 25:30 Pathology Deep Dive
- Transcytosis lets oxidised LDL pass through intimal cells.
- Macrophages engulf LDL, become foam cells, and secrete more inflammatory enzymes (LP-PLA₂, MPO).
- The process continues silently for years until the fibrous cap cracks.
25:30 – 33:30 hs-CRP Caveats & The Power of Albuminuria
Two-thirds of healthy people will spike hs-CRP 48 h after a flu shot.
Albumin in urine, though, is a direct proxy for endothelial damage: if your kidney filters (also lined by intima) leak protein, your arteries probably leak LDL.
33:30 – 40:00 Oxidation, Homocysteine & Methylation
Oxidation = inflammation. We counter it biologically by methylation; poor methylators accumulate homocysteine. A methylated B-complex (e.g., 5-MTHF) helps.
40:00 – 1:18:20 Audience Q & A (Highlights Only)
| Timestamp | Question | Short Answer |
|---|---|---|
| 44:30 | Optimal MPO & LP-PLA₂ cut-offs? | MPO < 400 pmol/L; LP-PLA₂ < 120–140 ng/mL (check your lab’s range). |
| 45:10 | Do I need fasting insulin if I’m already diabetic? | Yes—still shows how hard your pancreas is working. |
| 46:50 | Does chronic pain raise inflammation? | Indirectly, via cortisol spikes → higher blood sugar → insulin resistance. |
| 48:30 | Factor V Leiden screening? | Monitor inflammation too; clotting and plaque risk add together. |
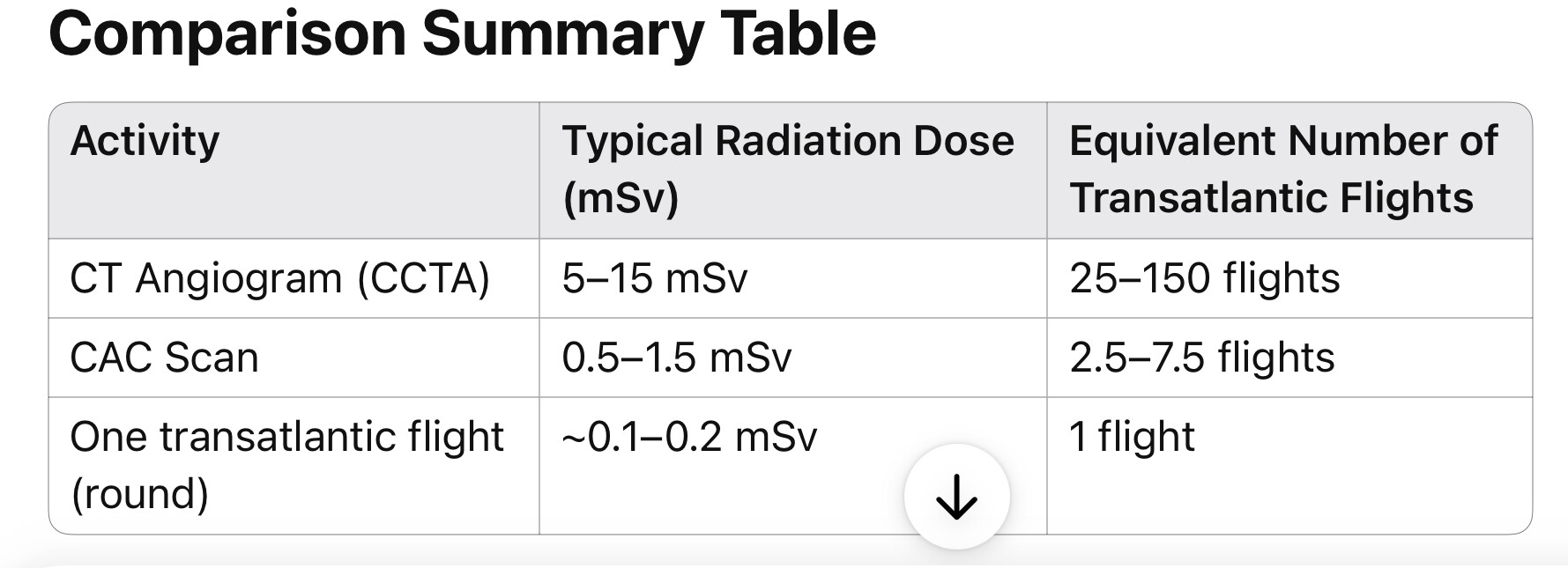
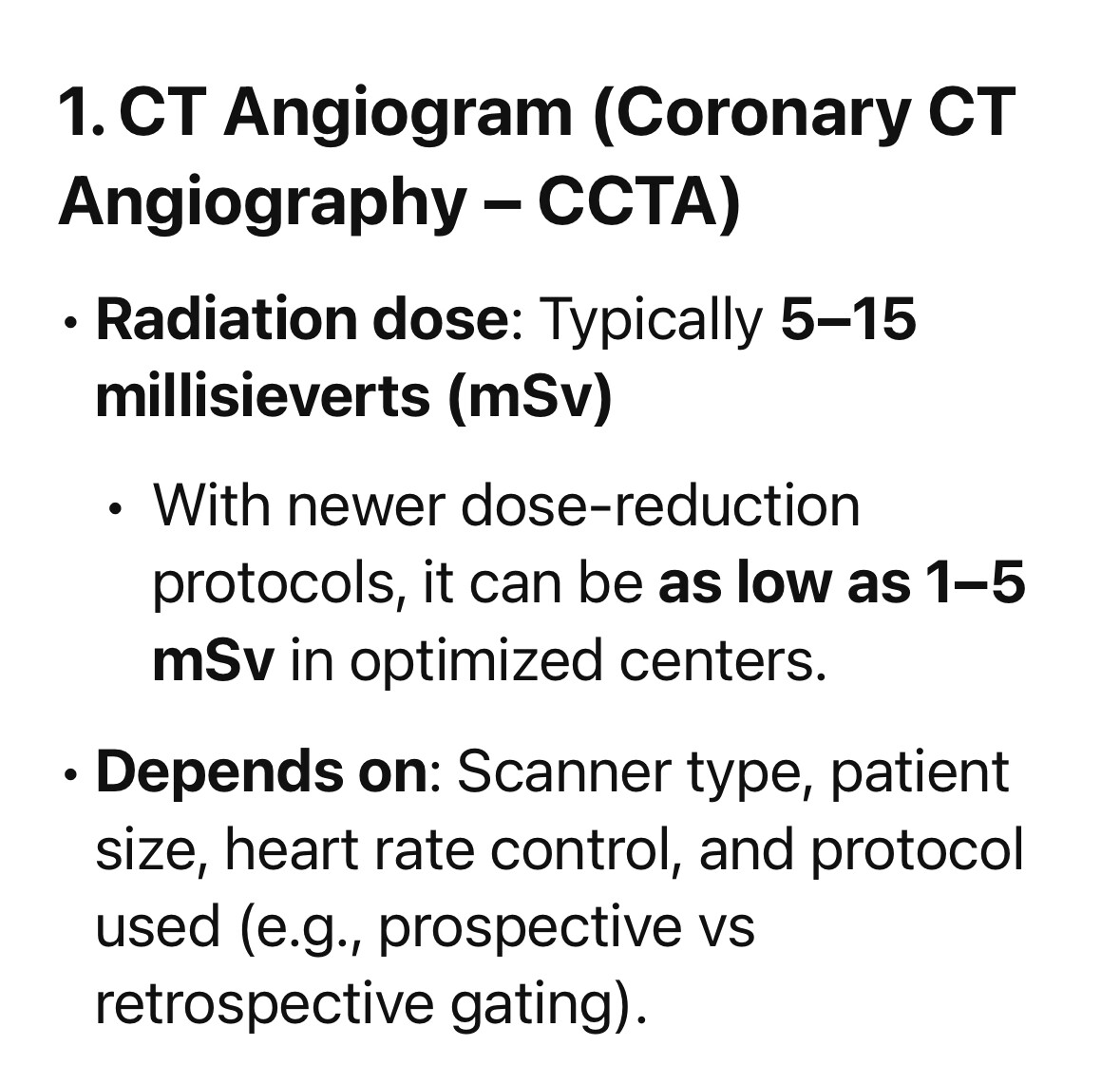
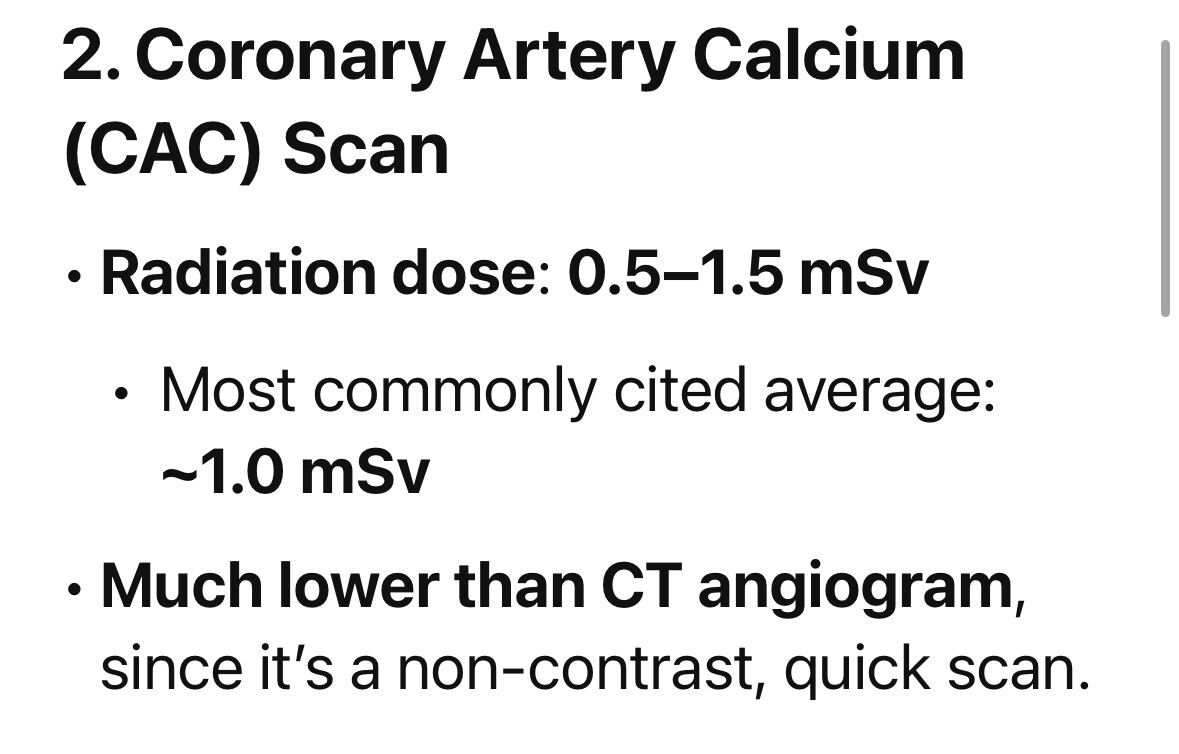
| 52:00 | Stress test vs CIMT vs CT angiogram? | CIMT is my go-to because it shows soft plaque and gives an “arterial age.” |
| 54:40 | Vitamin K2 while on Eliquis? | K2 is not the same as K1; generally safe, but confirm with your doctor. |
| 58:00 | Intermittent fasting and autophagy? | Solid evidence that skipping breakfast/time-restricted eating lowers inflammation. |
| 1:03:00 | Baby aspirin—still worth it? | In insulin-resistant patients, I still favor 81 mg despite recent headlines. |
| 1:06:00 | Femoral-IMT in addition to carotid? | Adds value only if carotid CIMT is pristine; <2 % reveal hidden plaque elsewhere. |
(Numerous other chat comments on vaccines, ivermectin, intro music, etc., have been omitted for brevity.)
1:18:20 Wrap-up
Thanks for your patience with the late start. We’ll keep balancing Medicare-clinic work with these weekly live streams. See you next time.
Note: Technical terms (intima, LP-PLA₂, MPO, etc.) are retained exactly as spoken. If you need a plainer-English glossary or want the entire verbatim chat section, just let me know!