Is elevated HbA1c a canary in the coal mine (indicates that blood glucose has been too high on average) or is it itself a problem? I.e. does high HbA1c mediate problems caused by high blood glucose or just indicate it?
Its the glucose that is the problem. Actually probably the peaks over 8 mmol/l
That’s what I would expect.
I’ve been in a similar boat with managing CVD risk and trying to stay proactive. I started statins a while ago after resisting them, and luckily, I haven’t had any side effects. Cutting back on saturated fat was a big shift for me, too, and I’ve found that exercise and managing stress have been just as important as the diet changes. I’ve heard good things about PCSK9 inhibitors and how they can lower LDL and help with plaque reduction, so I’m definitely curious to see where that goes, but like you, I’m waiting on more solid data before jumping in. It’s definitely a balancing act, but I think taking an active approach is key.
I was pointed to this “Research ArticleVolume 419132698January 15, 2025” reference by a talking head on YouTube, whom I will not mention because he constantly promotes supplements that he profits from. I don’t mind a little of this, but the frequent interruptions of his YouTube videos for promotion are excessive. IMO
In any case, the article is fine.
Is this the bottom line?
The tests that count in determining your coronary atherosclerosis risk are:
Total triglycerides
HDL particle size
“Increasing circulating levels of small HDL associated with diabetes with an OR of 1.37 and 95 %CI of (1.15–1.63). Among the HDL lipid components, phospholipids in small HDL associated with diabetes. On the contrary, lipid rich large (triglyceride) and extra-large (free cholesterol, phospholipids, and cholesterol esters) HDL associated with a lower risk of diabetes”
A1C
CRP
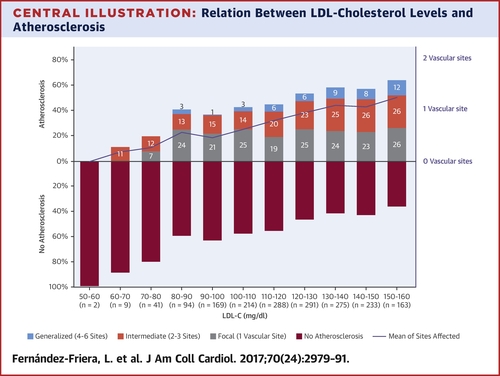
Many studies and social media doctors claim that there is no real correlation between LDL cholesterol and coronary atherosclerosis.
I previously thought that LDL particle size was a significant factor, when in fact, the HDL particle may be more predictive.
A Quest test from Ulta Lab that measures the particle size of HDL, LDL, etc.
https://www.internationaljournalofcardiology.com/article/S0167-5273(24)01320-2/fulltext
My mother was prescribed 80 mg of Atorvastatin after her heart attack and stents. Unfortunately, she is suffering from muscle weakness in her thighs and we believe it could be statin-related.
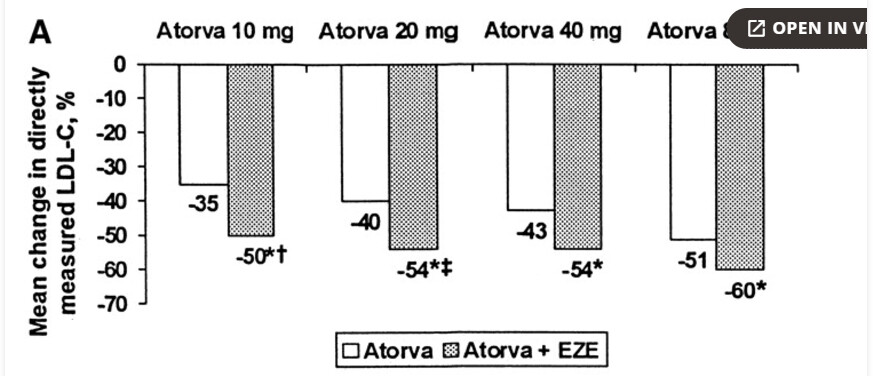
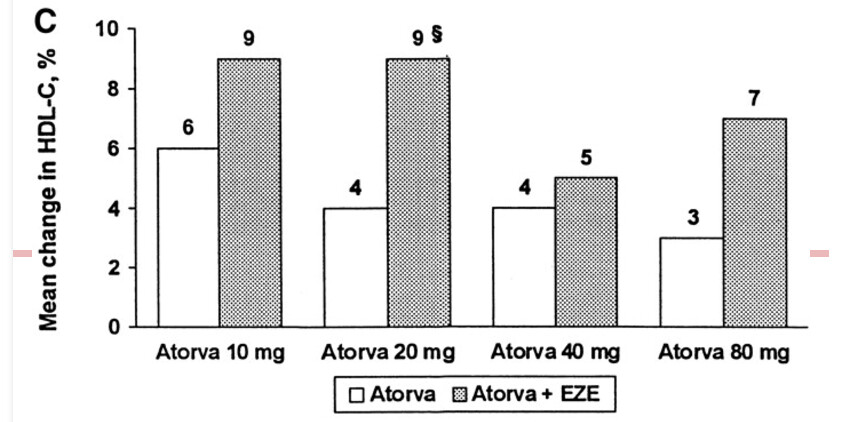
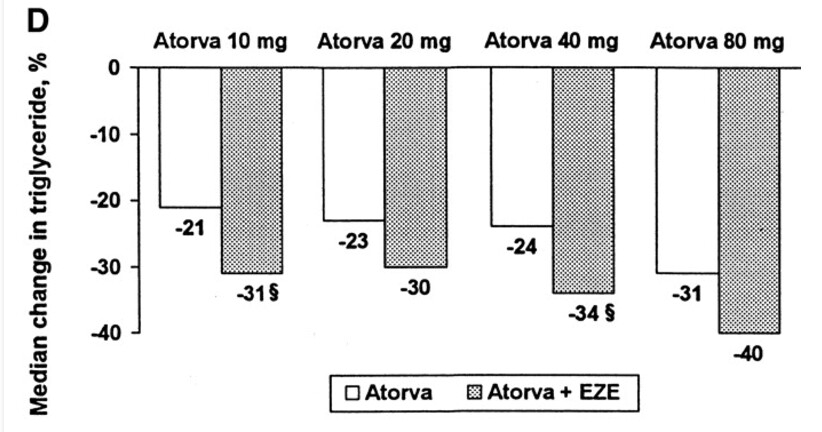
After researching the data here:
https://www.ahajournals.org/doi/10.1161/01.cir.0000068312.21969.c8
It seems that Atorvastatin 80 mg is just as effective at LDL reduction as 10 mg + Ezetemibe. The Ezetemibe + 10 mg increases HDL as a bonus. I’m going to ask the doctor to switch her to 10 mg of Atorvastatin and Ezetemibe.
Anything I’m overlooking here?
I would look into studies where secondary prevention is the focus of the research. The effect of statins in reducing heart attacks in individuals who already have heart disease is likely due to mechanisms other than lowering LDL-C levels (e.g., anti-inflammatory effects and plaque-stabilizing effects). Of course, LDL-C still plays a significant role over the long term.
However, as I understand it, even a small dose of statins provides the greatest benefits, for example, in reducing inflammation. Regarding the stabilizing effect, I’m not sure.
Personally, in that situation, I would probably ask for Atorvastatin 20 mg + Ezetimibe 5–10 mg
Possibly related, my relative switched to pitavastatin for similar challenges, and found no deleterious side effects.
Also inexpensive when purchased from India. (Compared to it not being covered at all, which the insurance co decided to do as of 2025.)
FWIW, I’ve switched from atorvastatin 10mg/day, to pitavastatin 4mg/day. I tolerated atorvastatin extremely well - basically no side effects and zero effects on any liver, kidney, glucose or other blood markes. However, atorvastatin started losing effectiveness as far as lowering LDL after a few years, and so I wanted to try pitavastatin. I picked pitavastatin for a variety of reasons, especially effectiveness against MACE and general CVD benefits. My PCP only offered to boost the dose of atorvastatin to control my LDL, and I thought this not effective. I therefore had to buy pitavastatin from Indian pharmacies, and the prices seemed very reasonable to me. I got Pivasta 4 from Zydus for $111 for 300 tablets.
I’ve stopped atorvastatin on Oct. 29/2024 and initiated the pitavastatin 4mg on November 1. So, it hasn’t been a month yet. I have so far not felt any effects whatsoever. I intend to get a lipid panel at the start of January 2025.
Before I decided on pitavastatin I’ve done a fair amount of research, and FWIW, there does seem to be less glucose perturbances, muscle pain, drug interactions and generally side effects with pitavastatin compared to atorvastatin, so that might be a consideration for some users. Meanwhile at least for CVD outcomes pitavastatin appears pretty stellar compared to most other statins.
The biggest cause of atheronic plaques is oxidized LDL cholesterol. Even when LDL is around 70, it begins to accumulate cumulatively in the vessel wall from the age of 20, and even if you lower LDL after a certain age, it may not have any effect. Therefore, it seems like a reasonable strategy to reduce LDL and Apo B levels to a reasonable level before the vascular wall accumulates with cholesterol.
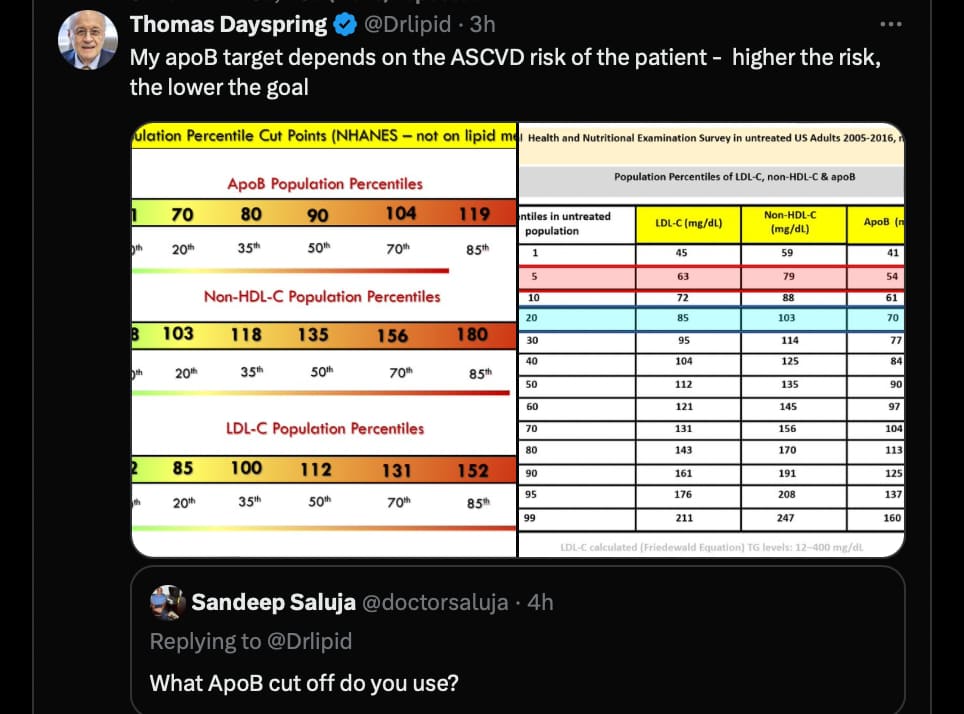
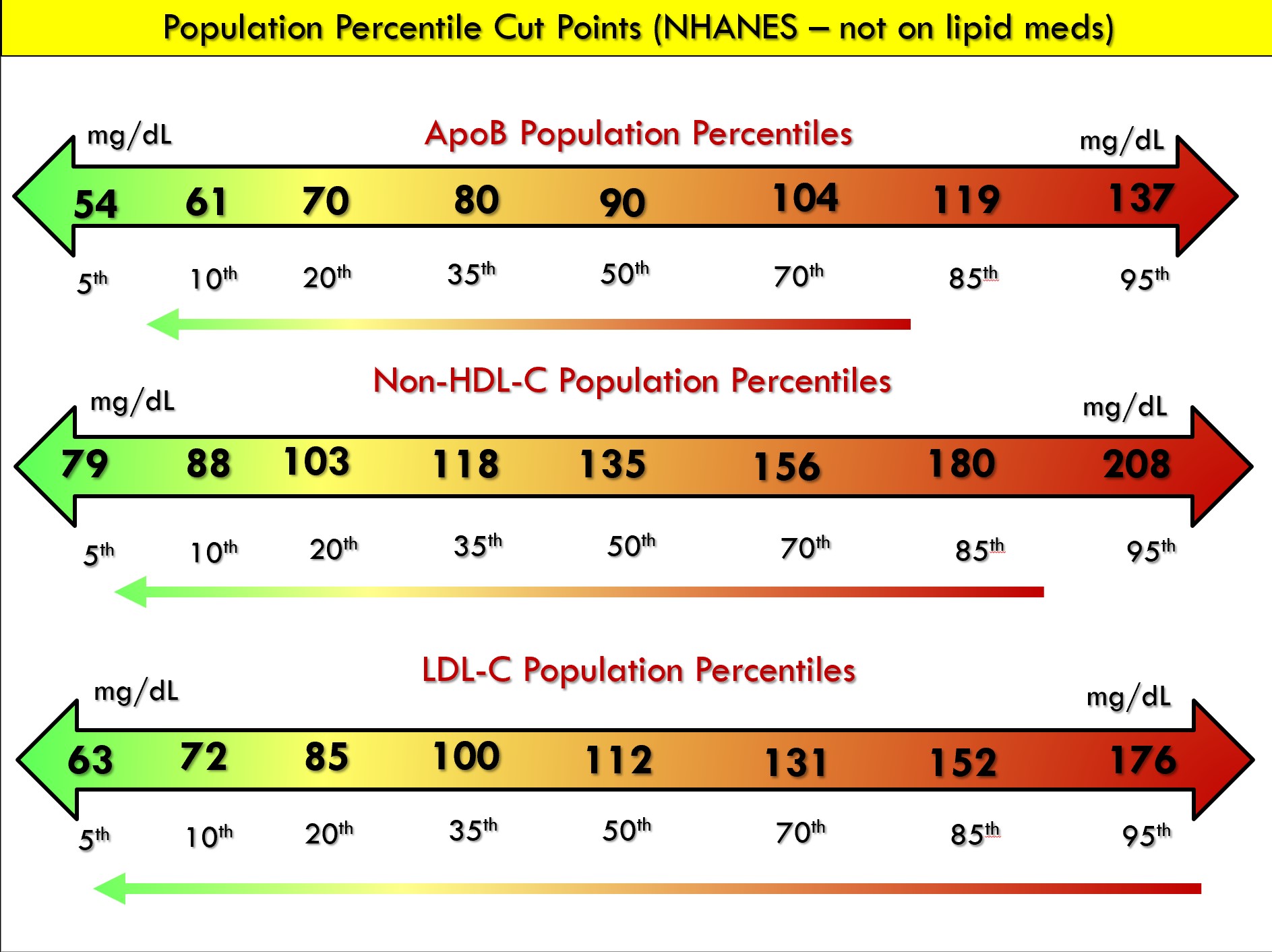
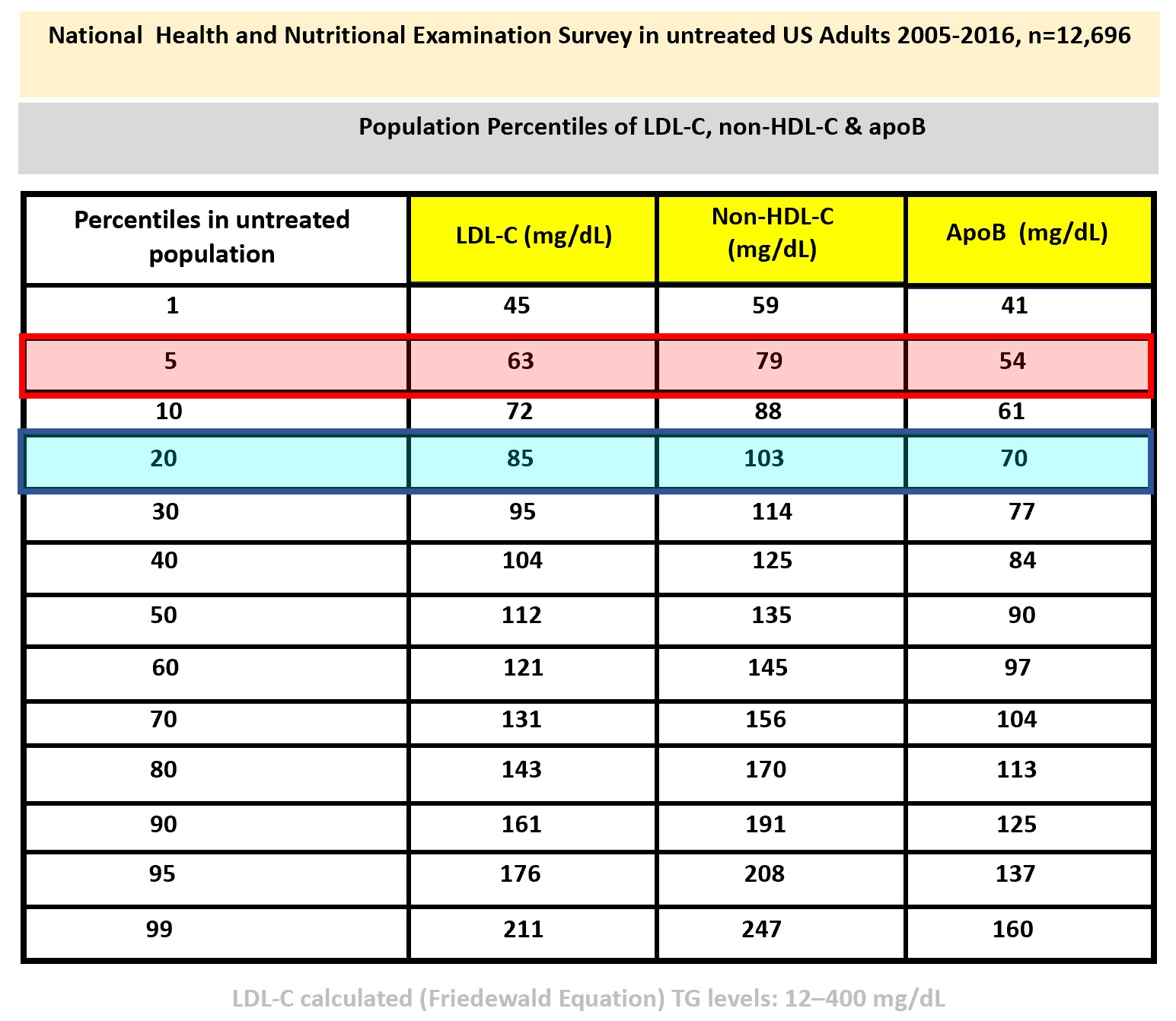
Thomas Dayspring is not an Immortalist / Don’t Die enthusiast or at least what I know, almost like Peter Attia. He is a lipidologist. If you have different goals you need a different approach I think or at least combine it. Lower in that case, of course.
I watched this entire video when it first came out and I have to say, it is probably the most comprehensive instructional video of exercise for longevity on the internet. Strongly recommend for anyone, even those of us who think we already knew a lot about exercise.
I have read quite a bit on this as well as watched some Youtube videos. Currently I think Dr. Ford Brewer has some of the most basic straight forward videos on this topic.
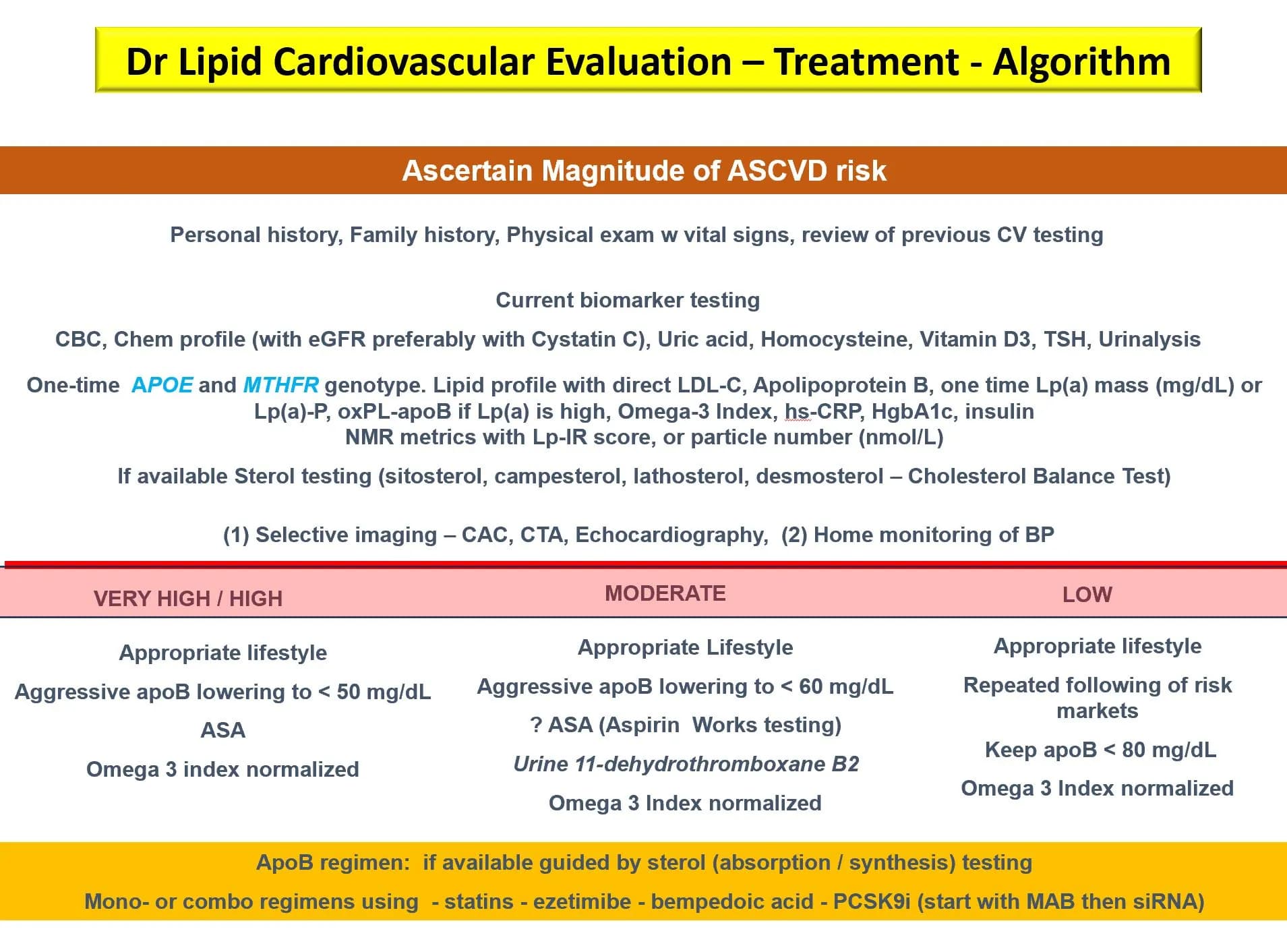
He recommends apoB < 70 mg/dL in most people and apoB < 50 mg/dL in “high-risk” people.
But his definition of “high-risk” is very broad and, I’m sure, includes at least a third of the population (high Lp(a), TG, HbA1c, insulin, homocysteine, hs-CRP, etc.):
Association of Plasma Omega-3 Levels With Incident Heart Failure and Related Mortalities 2024
In participants without HF at baseline (n=271,794), a generally linear inverse association was observed between omega-3 levels and incident HF during a median follow-up of 13.7 years. The risk was 21% lower in the highest quintile of omega-3 compared with the lowest quintile (hazard ratio, 0.79; 95% CI, 0.74 to 0.84; P<.001) in multivariable models.
In parallel models in participants with prevalent HF (n=1239), risk for all-cause and CV mortality were both reduced by approximately 50% comparing top to bottom omega-3 quintiles (hazard ratio, 0.53; 95% CI, 0.33 to 0.86; and hazard ratio, 0.50; 95% CI, 0.31 to 0.79, respectively; both P<.01).
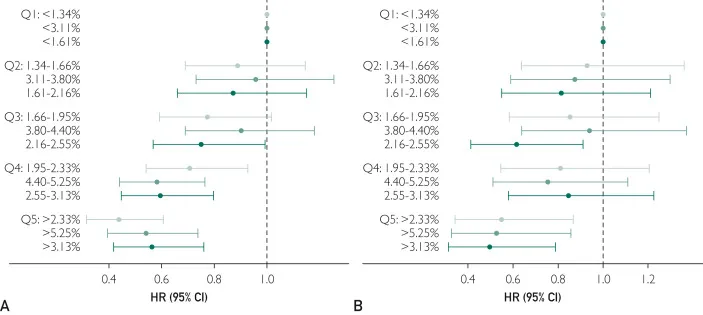
The two interesting charts:
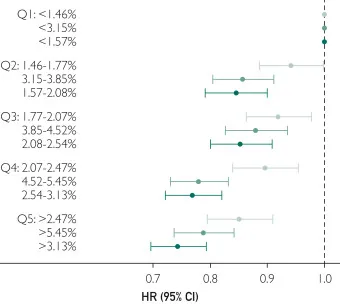
Figure 1. Forest plot illustrating the association between omega-3 plasma levels and the incidence of heart failure (HF). As omega-3 plasma levels increase, there is a concurrent decrease in the risk (ie, lower hazard ratio [HR]) of HF. Hazard ratios associated with docosahexaenoic acid (DHA) are shown in light gray, with total omega-3 in light green and non-DHA in dark green. Adjusted for age, sex, race/ethnicity, history of coronary heart disease, low-density lipoprotein to high-density lipoprotein cholesterol ratio, cholesterol medication, hypertension, diabetes mellitus, smoking status, alcohol consumption, level of education, exercise, body mass index, and waist circumference. Q, quintile.
Figure 2. Forest plots depicting the relationship between omega-3 plasma levels and all-cause mortality (A) and cardiovascular mortality (B). As omega-3 plasma levels increase, there is a corresponding decrease in the risk of all-cause mortality (A) and cardiovascular mortality (B). Hazard ratios associated with DHA are shown in light gray, with total omega-3 in dark green, and non-DHA in black. Adjusted for age, sex, race/ethnicity, history of coronary heart disease, low-density lipoprotein to high-density lipoprotein cholesterol ratio, cholesterol medication, hypertension, diabetes mellitus, smoking status, alcohol consumption, level of education, exercise, body mass index, and waist circumference. Q, quintile.
So to be in the top quintile, you need:
- Serum DHA: >2.47%
- Serum total omega 3: >5.45% (
 This is NOT the omega 3 index as the omega 3 index looks at RBC and not serum
This is NOT the omega 3 index as the omega 3 index looks at RBC and not serum  )
) - Serum non-DHA: >3.13%
Regarding non-DHA, they note:
In our study, when comparing the plasma levels of DHA, non-DHA, and total omega-3 as exposure markers, associations with risk for HF were somewhat stronger for non-DHA than DHA. For the mortality outcomes, differences in HRs were reasonably similar with all 3 metrics. An interlaboratory experiment (see Patients and Methods) confirmed that the strongest predictor of non-DHA omega-3 levels was EPA (R2=46.8%), while neither alpha-linolenic acid nor docosapentaenoic acid were statistically significant predictors (P>.05 in both cases) of the non-DHA omega-3 level. Thus, it appears (although only inferred) that a higher EPA level may have been more directly linked to the lower incidence of HF than a higher DHA level. This finding aligns with the results from the Multi-Ethnic Study of Atherosclerosis (MESA), which reported that higher plasma EPA levels were significantly associated with reduced risk for HF after 13 years of follow-up.
Context matters, if you asked him that you wanted to try to avoid atherosclerotic disease forever he would probably say to target 30 mg/dl or lower.
There are barely any side effects of ezetimibe and PCSK9 inhibitor.
That must mean these are true longevity drugs. And obicetrapib might join that camp soon as well.