Which statin have you tried before? At which dose?
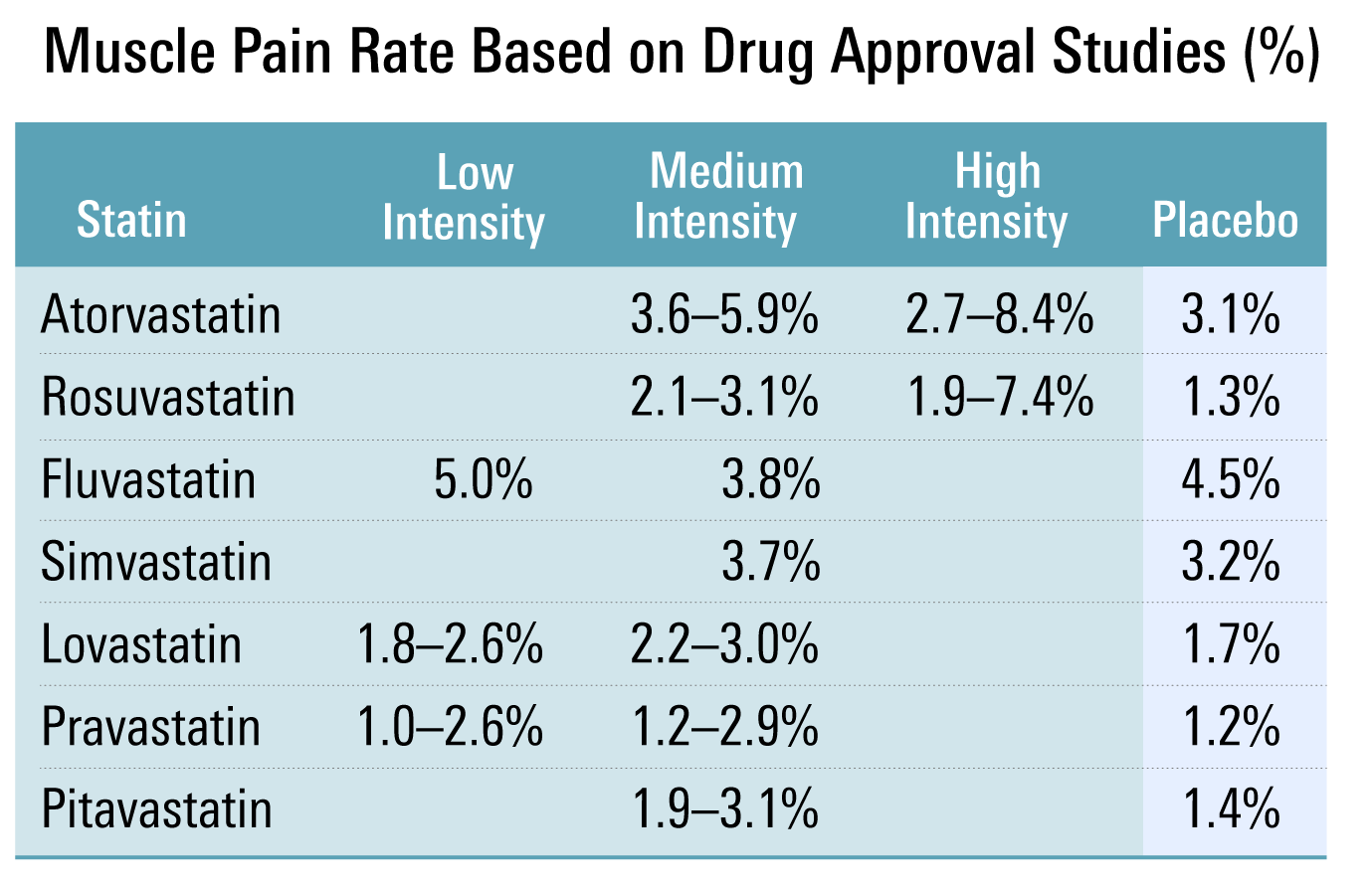
Statin intolerance is highly dependent on the type of statin and the dose used:
Statin Intolerance: the Clinician’s Perspective 2015:
In patients with statin intolerance , very low doses of statins administered via an altered dosing regimen should be attempted and, if tolerated, should be gradually increased to achieve the highest tolerable doses. With this cautious approach, the majority of patients are able to tolerate at least some degree of statin therapy.
Statin Intolerance 2015:
The intolerance can be either partial (ie, only some statins at some doses) or complete (ie, all statins at any dose).
Before considering the use of a second-line alternative drug, patients should try statin rechallenge, alternative regimens, doses, or types of statins. In most cases, rechallenge with a statin after a brief period of drug discontinuation (“drug holiday”) can be successful. In a study of 11 124 patients in whom statins were discontinued at least temporarily because of clinical events or symptoms believed to have been caused by statin use, 92% of those who were rechallenged were still taking a statin 12 months after the statin-related event.
NLA scientific statement on statin intolerance: a new definition and key considerations for ASCVD risk reduction in the statin intolerant patient 2022
To classify a patient as having statin intolerance, a minimum of two statins should have been attempted, including at least one at the lowest approved daily dosage.
To identify a tolerable statin regimen it is recommended that clinicians consider using several different strategies (e.g., different statin, dose, and/or dosing frequency).
An acceptable statin treatment regimen can be identified for most patients with statin intolerance which may require a different dose, statin, or dosing schedule.
For instance, I know someone intolerant to atorvastatin who uses rosuvastatin without any problem. See also:
My guess is that rosuvastatin 2.5 mg and atorvastatin 5 mg are identical to placebo in terms of tolerance at the population level, of course this might differ at the level of the individual. Pitavastatin seems also very interesting (check papers about it).
(By the way, I don’t say you should use a statin, I’m just commenting on their tolerability.)