Correct me if I’m wrong but you switched to empa and did not experience such issues, right? or maybe was at @admin who said that?
Reason for my chime in, I’m about to place my first order of empa.
I switched to Empa because I had some sort of “exhaustion” side effect with Cana. its a pretty rare side effect, from my research, so I moved to Empa. Empa has been fine with no obvious side effects. But for anyone else, this likely is not a reason for Empa over Cana.
Yes, I have switched to empa with no discernable side effects.
I’m not sure it is the opposite - we both acknowledge the following I think
-
Cana may have some more risks on diabetic patients based clinical data
-
Cana but no other SGLT2i or other SGLT1i has been tested in ITP multiple times and each time been successful
-
Cana is both SGLT2i and SGLT1i and the other SGLTi’s that people are taking her on the forum are generally “pure” SGLT2i
-
We cannot know for sure if the SGLT1i part was needed for the Cana ITP longevity results to have been consistently reached
Perhaps the summary is
Cana in “expected” space is perhaps higher risks and higher longevity benefit, while E and D might have longevity benefits and might be safer (if you are a diabetic).
The gut does seems to be involved with a lot of longevity things - including in the case of Acarbose and it seems like that may be one of the big differences:
SGLT1 is primarily expressed in intestinal epithelium, whose inhibition reduces dietary glucose uptake, whilst SGLT2 is highly expressed in kidney regulating glucose reabsorption.
And/or stopping the update might be different that regulating reabsorption down stream
Does anyone have access to:
Does anyone know which SGLTi Peter Attia uses? and/or which one his clinic prefers to prescribe?
—
Also found the below interesting with respect to above:
Summarizing what we know about canagliflozin:
- We don’t know whether the positive effect of canagliflozin is due to its impact on glucose, SGLT2, or SGLT1
- The literature is showing, for example… effect on tumors specifically, and other things like heart attacks, independent of whatever’s happening in terms of glycemic control
- The shortest, simplest explanation—that the benefits are due to canagliflozin’s effect on glucose—may not be right. — “There are other ideas that deserve a lot of exploration.”
- Peter reiterates his excitement around canagliflozin: “We are very excited about this class of drugs clinically in our practice; the cardioprotection, renal protection, obviously the glycaemic benefits are all pretty exciting.”
I wasn’t clear enough: I think that besides higher risks, cana might have lower longevity benefits. Indeed, canagliflozin does not seem to perform significantly better than empagliflozin and dapagliflozin in clinical trials and longitudinal studies for T2D, CKD, HF, etc.
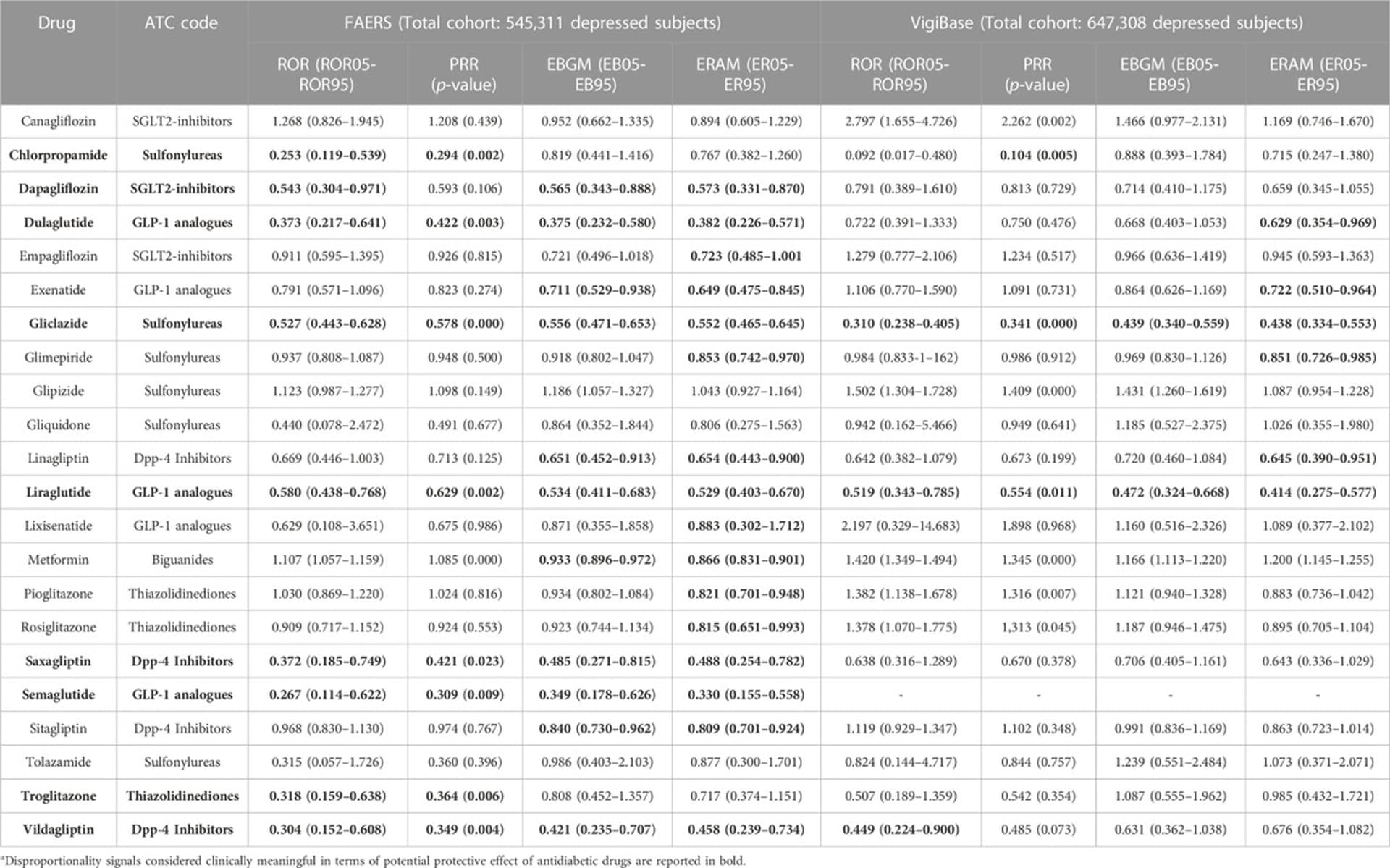
Here’s one example among many others: cana seems to be associated with an increased risk of depression while dapagliflozin slashes depression risk by 2: The potential antidepressant effect of antidiabetic agents: New insights from a pharmacovigilance study based on data from the reporting system databases FAERS and VigiBase 2023
It’s just one longitudinal study, so it does not prove much, but there are several signals like this. I have yet to find one study where canagliflozin strongly outperforms dapagliflozin and empagliflozin.
It’s also interesting to look at the number of clinical trials currently recruiting:
- cana: 15 studies
- empa: 97
- dapa: 109
It seems that researchers all around the world are 10x more excited by empagliflozin and dapagliflozin than by canagliflozin.
We actually know for sure that SGLTi benefits are not due primarily to their effect on glucose: in longitudinal studies, when compared to other glucose-lowering drugs such as DPP4, they perform way better: Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitors vs. Dipeptidyl Peptidase-4 (DPP4) Inhibitors for New-Onset Dementia: A Propensity Score-Matched Population-Based Study With Competing Risk Analysis 2021
Similarly, SGLTi are approved for CKD and heart failure, whereas other glucose-lowering drugs are not.
So, for sure, they have systemic effects in addition to their glucose-lowering properties. This is well explained in these recent overviews:
Actually, I’ve just found this paper which may negate the above I’ve just said ![]()
Meanwhile, a retrospective cohort study conducted in Taiwan showed consistent results with our findings with 12,681 new users of dapagliflozin or empagliflozin, i.e., similar risks of composite cardiovascular outcomes and a significantly lower risk of heart failure in dapagliflozin users [36]. Cardiovascular death in this Taiwanese study was also lower in the dapagliflozin group (HR 0.54, 95% CI 0.14–2.12). […] it is intriguing to note that significant differences between users of dapagliflozin and empagliflozin were observed only for these two outcomes. This may allude to intrinsic disparities between the two drugs and could lead us to posit that dapagliflozin may exert more pronounced pleiotropic effects on heart failure outcomes than empagliflozin. For example, different neurohormonal responses might be one of the possible mechanisms. A previous study revealed that empagliflozin significantly increased plasma aldosterone and noradrenaline levels; however, dapagliflozin did not. It was also noted that the change in plasma volume is a key mediator in reducing cardiovascular death among users of SGLT2 inhibitors. Taken together, different neurohormonal responses and the concomitant reductions in plasma volume might synergistically contribute to the further decrease in the risk of heart failure-related events and cardiovascular death in dapagliflozin users. On the other hand, neurohormonal responses may not affect ischemic endpoints such as MI or ischemic stroke, as SGLT2 inhibitors have been found to be independent of pathways governing arterial thrombosis. This is further supported by the pronounced advantages observed in women. Specifically, in our subsequent analysis, the cardiovascular benefits were evident only in women > 50 years. Although individual menopausal status could not be noted, women > 50 years, who were mostly in their peri- or post-menopausal stage and, hence, more susceptible to changes in neurohormones and plasma volume, would have benefited more from dapagliflozin and showed improved cardiovascular outcomes. Secondly, the approximate 2.5-fold greater affinity for SGLT2 and six-fold greater affinity for SGLT1 exhibited by dapagliflozin compared to empagliflozin might have contributed. Currently, the benefits of adding SGLT1 to SGLT2 inhibition are receiving attention. A study with Mendelian randomization data revealed that patients with missense mutations in the SGLT1 gene had reduced risks of heart failure and death. Recent clinical trials, SOLOIST (effect of sotagliflozin on cardiovascular events in patients with type 2 diabetes post worsening heart failure) and SCORED (effect of sotagliflozin on cardiovascular and renal events in patients with type 2 diabetes and moderate renal impairment who are at cardiovascular risk), also raised the possible advantage of additional SGLT1 inhibition for cardiovascular outcomes. Accordingly, the higher SGLT1 and SGLT2 affinity of dapagliflozin compared to that of empagliflozin might contribute to the lower risks of heart failure-related events and cardiovascular death in our study. In addition, several studies have suggested that the SGLT2-independent effects of this drug class, which are presumed to take place in the myocardium, are likely attributed to off-target effects, given the notably low levels of SGLT2 in cardiac cells. Further investigations focusing on differences in off-target effects between dapagliflozin and empagliflozin are needed.
So I still think that dapa and empa are better than cana. But maybe sotagliflozin does SGLT1 inhibition “better” than cana and is even better than all others. Sotagliflozin was only approved in the US in 2023. So it will take time to have good data on sotagliflozin vs cana, dapa, and empa… So far the only comparison we have is this clinical trial of empa vs sota for 8 weeks: identical results except after breakfast where sota is more potent (better glucose, insulin, GIP, and GLP-1 AUCs): Metabolic, Intestinal, and Cardiovascular Effects of Sotagliflozin Compared With Empagliflozin in Patients With Type 2 Diabetes: A Randomized, Double-Blind Study
I don’t mind if cana is better for heart disease since that can already be prevented with statins etc. I don’t tend to pay much attention to heart disease for that reason. Possible better mood with dapa is a big plus, and as well if it’s better in other ways.
It makes sense that SGLT2i’s increase risk of UTI’s, since the sugar is dumped in urine.
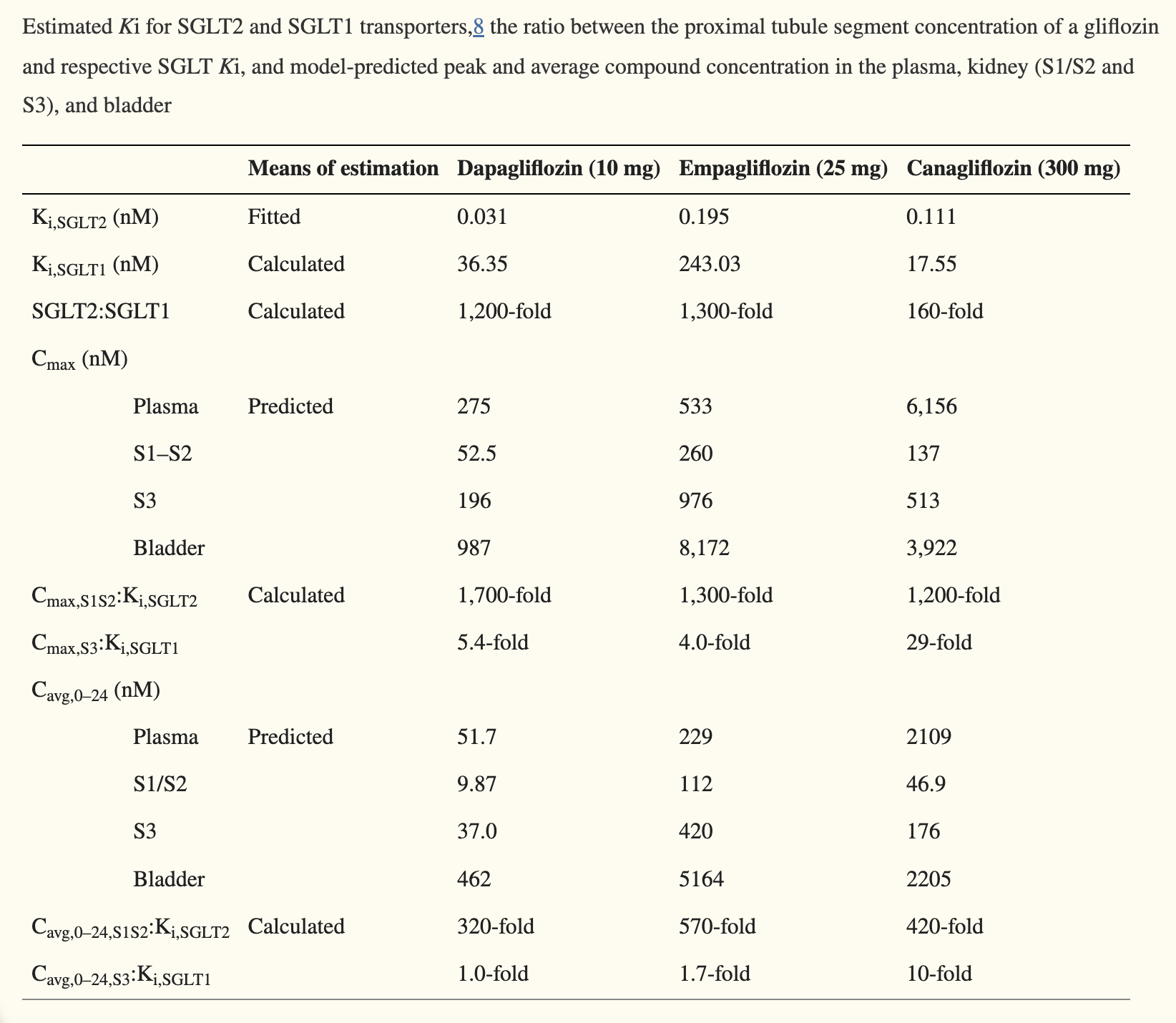
Is this saying that both dapag and empag have sglt1 effects? And that dapag is stronger for both SLGT2 and sglt1?
I thought only canag and sotag had sglt1 effects.
I don’t understand either, but I assume nothing is black or white:
Here’s another paper we already cited previously: “At approved doses, canagliflozin, but not dapagliflozin or empagliflozin, inhibits renal SGLT1, which may reconcile the differences in clinical efficacy and safety among gliflozins. […] At approved doses, SGLT1 inhibition by canagliflozin but not dapagliflozin or empagliflozin contributed to ~ 10% of daily urinary glucose excretion.” (Differentiating the Sodium‐Glucose Cotransporter 1 Inhibition Capacity of Canagliflozin vs. Dapagliflozin and Empagliflozin Using Quantitative Systems Pharmacology Modeling )
Im having a bit of trouble following
You cite
Currently, the benefits of adding SGLT1 to SGLT2 inhibition are receiving attention. A study with Mendelian randomization data revealed that patients with missense mutations in the SGLT1 gene had reduced risks of heart failure and death
Why does that not argue that Cana (and perhaps dapa if it in fact has meaningful SGLT1i) is not favorable based on the Mendelian causal data of SGLT1?
—-
Separately, I feel that you have not a single time addressed or commented on that the only SGLTi drug that we have proof of longevity from the gold standard ITP (more than once) - median and maximum life extension - is from Cana - and hence we have to be open to that SGLT1 inhibition may be crucial to mammalian life extension…?
Is there something incorrect with the logic in the last statement/question?
I think it helps with other forms than heart disease that’s vessel based issues / cardiovascular disease? So that it still something that our aggressive ApoB lowering won’t solve (I’m on PCSK9i and about to add Eze - and agree with you on driving ApoB to the bottom).
Also most mortality benefits from SGLT2i in humans are from (often obese) diabetics - so while compelling conjectures can be made for longevity/life extension, the only causal data on life extension in humans - which you have called for is what matters most - if from Mendelian randomization, including that SGLT1i is linked to less mortality
Combined with only experimental causal link to life extension in mammals is the ITP with Cana (and hence multiple centers, across more than one ITP)
Seems to me that one cannot say that above does not mean that we have to at least weigh
- whether SGLT1i is needed,
- whether it might be that SGLT1i alone and not the SGLT2i at all is needed, or
- whether it needs to be a similar mix of 1&2 inhibition that Cana has is needed?
Am I missing something here @A_User - above seems to be fully consistent with the frameworks you have suggested we use when making decisions.
Above of course has to be weighed against any disease data one cares about outside of longevity and life extension and also against any side effect risk profiles.
But one cannot not weigh in one’s equation that (i) Cana is the only one where we have casual longevity in (gold standard) mammalian studies and (ii) SGLT1i was part of that and SGLT1i has Mendelian support against mortality.
This “may” be true, but really the only rigorous, full lifespan testing information we have on any of the 'flozins is with Canagliflozin and mice in the ITP study (Cana is the only flozin that is proven to be lifespan extending right now). So we can’t be sure that the other flozins lengthen life in mammals.
Given the data we have on the other flozins it seems likely that they offer the the same benefits, (or more), but you can never be sure until you run the study.
I’m not disagreeing with you, but just putting in a word of caution about getting too far ahead of the data, and just encouraging a little skepticism in going beyond the data.
Is the mechanism of action really on blood glucose? The result seem so powerful in preventing death among HF patients:
Sotagliflozin in Patients with Diabetes and Recent Worsening Heart Failure
https://www.nejm.org/doi/full/10.1056/NEJMoa2030183
Wouldn’t drugs with a similar decrease in blood glucose have a similar effect if so?
The effect is most certainly not from blood glucose control, when it comes to humans at least and HF.
Whereas SGLT2 inhibitors are effective glucose-lowering agents, the efficacy on heart failure is unlikely related to improvements in glucose lowering per se. Hyperglycemia itself has been shown to be a weak risk factor for cardiovascular disease (65). In addition, the rapid efficacy noted (within days of treatment initiation) is difficult to reconcile with a glucose-lowering effect. Furthermore, the differences in glycemic control in the cardiovascular outcome trials were small (in an effort to fulfill the glycemic equipoise principle of the trials), and post hoc analyses from trials suggested that baseline A1c or changes in A1c were not associated with any treatment modification with SGLT2 inhibitors (65). Definitive proof of this concept emerged from the DAPA-HF trial wherein the efficacy of dapagliflozin was entirely consistent in those with and without diabetes. Even in those without diabetes, efficacy was similar in those with pre-diabetes or impaired glucose tolerance compared with in those who were truly euglycemic. When studied continuously, using fractional polynomial analyses, baseline A1c was unrelated to the efficacy of dapagliflozin to reduce heart failure and mortality in DAPA-HF. In addition, in experimental models of heart failure, the benefit of SGLT2 inhibition has been observed independent of diabetes or hyperglycemia (60,66,67).
Really strange drug, but nice to learn about something new, the flozin drug class. Pee out glucose, but it’s not the peeing out glucose that helps for heart failure by reducing all cause mortality, okay.
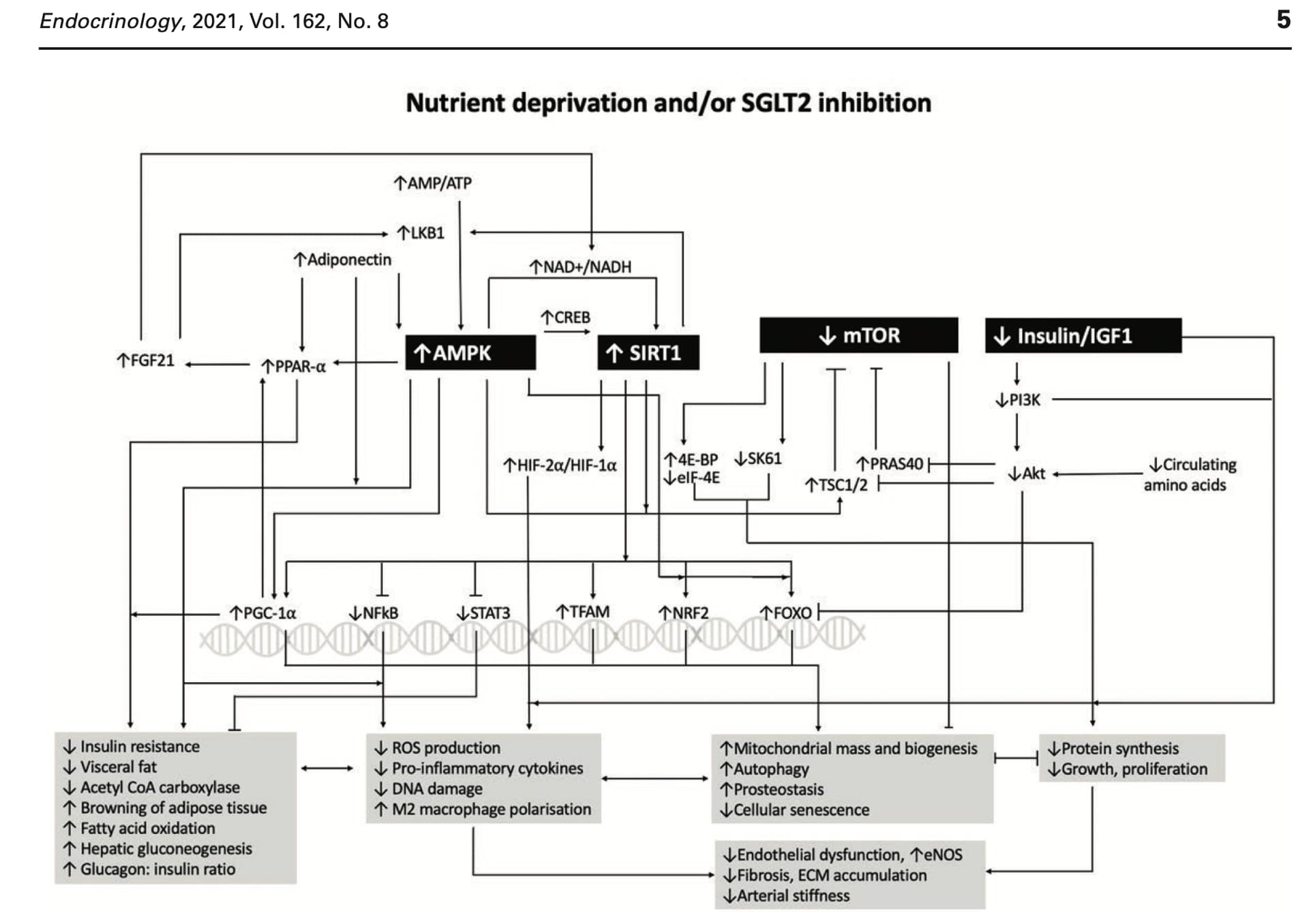
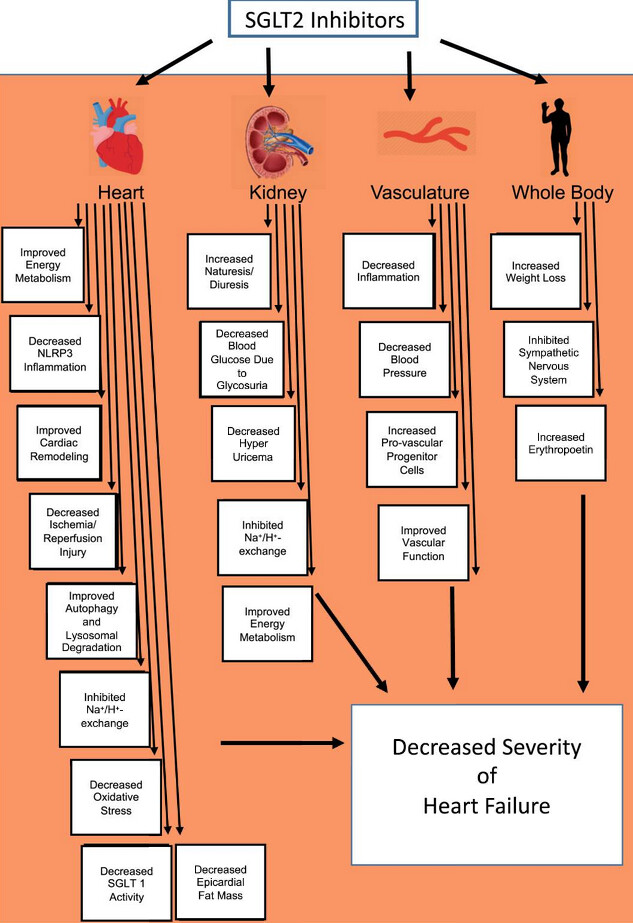
My guess since 2021 has been not only/not mostly, it goes beyond that in many ways. See for instance
and in general skim this paper (that the figure above is from)
SGLT2 Inhibitors as Calorie Restriction Mimetics: Insights on Longevity Pathways and Age-Related Diseases
and
- Critical Reanalysis of the Mechanisms Underlying the Cardiorenal Benefits of SGLT2 Inhibitors and Reaffirmation of the Nutrient Deprivation Signaling/Autophagy Hypothesis - see www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.122.061732
And here are from the NIH and NIA’s ITP:
- The gold standard Interventions Testing Program (ITP), supported by the NIH/National Institute on Aging (NIA), tests the effects of drugs on life span. ITP studies use annual cohorts of genetically heterogeneous mice (UM-HET3) equally distributed among 3 testing sites. Here is the first paper on the results with Canagliflozin.
and
and (might be of extra interest for @adssx given interest in neuro protection):
Your last statement is perfectly logic. Canagliflozin is mostly an SGLT2 inhibitor and also partially SGLT1 inhibiting. From here one can think “So it’s possible that its longevity properties are partially derived from SGLT1 inhibition” or “It could be that SGLT1 inhibition is not that beneficial and that SGLT2 inhibition only is better”. My opinion is neither of these two assertions: I don’t know (and as of today, no one knows). But I know that in most retrospective longitudinal studies looking at different outcomes (depression, dementia, diabetic retinopathy, etc.) canagliflozin is not significantly better than dapagliflozin and empagliflozin. So my bet is that dapagliflozin or empagliflozin would perform better than canagliflozin if they were tested in the ITP. But that’s a pure guess. It’s possible that sotagliflozin would perform even better. That’s all what I say.
Thanks - this makes sense, I see what is known and what is a conjecture/feeling.
Hopefully more data will help us over time.
Unfortunately I’m afraid the ITP won’t test another flozin and clinical trials rarely compare two active substances. So we may just have a few rodent studies here and there on some biomarkers. And longitudinal data on humans in a few years for sotagliflozin.
We may see epigentic clock measures applied in people taking SGLTi’s
while it would not covered everything that would help provide additional support on whether their are longevity effects beyond anti disease effects
hopefully we can also see more Mendelian randomization studies come out over the next 2-3 years and those types of papers are growing in frequency
And if AgelessRx and perhaps others run small trials we’ll have that
And if interest grows in the direction of what it has done for rapa (and Met and Acar), perhaps we’ll be able to puzzle together some of the answer from a lot of N=1 experiences.
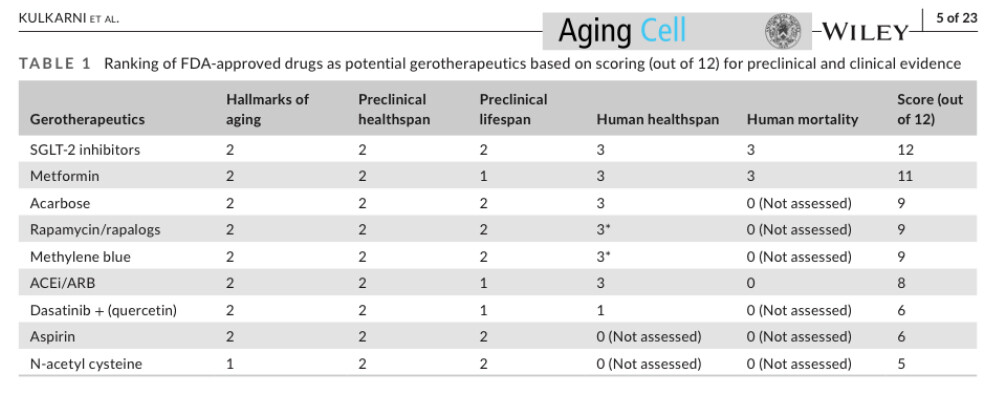
The main guy behind TAME ranked SGLT higher than Met in attractiveness for a gerotheraputic - so perhaps we can eventually see a TAME like trial for SGLTi:
-
Geroscience-guided repurposing of FDA-approved drugs to target aging
- See e.g. the intro and first table