Yes, but what is interesting is that rates of new cancer and rates of deaths from cancer are divided by two among SGLT2is users compared to other anti-diabetic drugs. So it’s probably not glucose-related. SGLT2is only have a modest effect on glucose levels anyway.
Wow, that is huge. Depending on the data, that could be one of the biggest reasons to consider SGLTi in healthy individuals
With the current medications available, getting to 100-110 seems fairly realistic even for couch potatoes.
Can you share more about this!
(Found some potentially different synthesis below)
—
Meta analysis does not seem to agree with meaningful reduction
Seventy-six trials encompassing 116,375 participants were selected. Overall risk of bias was low. SGLT2 inhibitors did not reduce/increase the overall risk of cancer (RR, 1.03; 95% confidence interval [CI], 0.96–1.10) and cancer mortality (RR, 0.99; 95% CI, 0.85–1.16). SGLT2 inhibitors likely result in little to no difference in the risk of breast (RR, 1.01; 95% CI 0.77–1.32) and bladder cancers (RR, 0.93; 95% CI 0.71–1.21). Trial sequential analysis provided evidence that the sample size was sufficient to avoid missing alternative results.
Specific cancers (MR studies):
For genetic evidence, genetically proxied SGLT2 inhibition reduced the risk of overall (odds ratio=0.56, 95%CI=0.38 to 0.82), advanced (OR=0.52, 95%CI=0.27 to 0.99) and early-onset (OR=0.27, 95%CI=0.11 to 0.72) prostate cancer.
In primary analysis, SGLT2 inhibition was associated with reduced risk of bladder cancer (OR: 0.98, 95% CI: 0.97-0.99) per unit lowering of HbA1c level. A protective association was also observed for prostate cancer with odds ratio = 0.31 (95% CI = 0.21-0.47). However, we did not discover a causal relationship between SGLT2 inhibition and kidney cancer (OR: 1.00, 95% CI: 0.99-1.00).
Here divided by 5: Canagliflozin - Another Top Anti-aging Drug - #334 by adssx
Here cancer‐related mortality divided by 2: Canagliflozin - Another Top Anti-aging Drug - #390 by adssx
Here divided by 2: Canagliflozin - Another Top Anti-aging Drug - #861 by adssx
Also, even more here for dapagliflozin: Effects of novel SGLT2 inhibitors on cancer incidence in hyperglycemic patients: a meta-analysis of randomized clinical trials 2022
Our meta-analysis showed that SGLT-2 inhibitors were significantly associated with an overall reduced risk of cancer as compared to placebo (RR = 0.35, CI 0.33–0.37, P = 0.00) with a particular effectiveness for dapagliflozin and ertuglifozin (RR = 0.06, CI 0.06–0.07 and RR = 0.22, CI 0.18–0.26, respectively). Network Medicine approaches may advance the possible repurposing of these drugs in patients with concomitant diabetes and cancer.
All the above in diabetic patients. Might not translate to normoglycemic people.
Here’s a more recent meta-analysis of clinical trials: Sodium-glucose cotransporter 2 inhibitors and cancer: a systematic review and meta-analysis 2024
Compared to the placebo SGLT2 inhibitors did not significantly increase the overall incidence of cancer (RR 1.01; 95% CI 0.94–1.08; p = 0.82).
However, dapagliflozin did significantly reduce the risk of bladder cancer by 47% (RR 0.53; 95% CI 0.35–0.81; p = 0.003).
Dapagliflozin reduced the risk of respiratory cancer by 26% (RR 0.74; 95% CI 0.55–1.00; p = 0.05). SGLT2 inhibitors (particularly mediated by dapagliflozin and ertugliflozin but not statistically significant) were associated with a greater risk of renal cancer than the placebo (RR 1.39; 95% CI 1.04–1.87; p = 0.03).
Trials last about 1y. So, I think it’s normal not to see effects. The finding for renal cancer might be concerning but cohort studies do not corroborate it: Sodium–Glucose Cotransporter 2 Inhibitors and Risk of Bladder and Renal Cancer: Scandinavian Cohort Study 2022
Use of SGLT2 inhibitors, as compared with GLP-1 receptor agonists, was not associated with a statistically significant increase in risk of bladder cancer (adjusted HR 0.88 [95% CI 0.59–1.31]) or renal cancer (adjusted HR 1.09 [95% CI 0.73–1.63]) (Table 1). In additional analyses, the adjusted HR did not increase with time since cohort entry (Table 1). In several sensitivity analyses, including those with adjustment for additional variables such as smoking and glycated hemoglobin, the findings did not differ materially from those of the main analyses (Table 1).
Given that MR studies did not find much and that dapagliflozin seems to be an outlier (in both clinical trials and longitudinal studies), the potential positive effects might be off-target and might not be class effects.
The SGLT1 vs 2 debate is still on: The SGLT2 inhibitor canagliflozin, but not dapagliflozin or empagliflozin, ameliorates vascular calcification in a mouse model of nephrocalcinosis 2024
One more potential mechanism: The effect of dapagliflozin on anemia in patients with CKD 2024
The use of dapagliflozin for eight months resulted in a significant elevation in hemoglobin levels in patients with CKD. Further studies can explore of better understanding of the effect and confirm the mechanisms that explain this finding. Elevation of hemoglobin with SGLT2is may be closely linked to the reduction of cardiovascular mortality and heart failure.
Compared to non-SGLT2i cohort, patients who received SGLT2i had a significantly lower risk of MD (adjusted hazard ratio = 0.70, 95%CI = 0.66–0.75).
We found that SGLT2is has a strong protective effect against MD in patients with diabetes. SGLT2is may have benefits beyond glycemic control in patients with DR. However, additional clinical and experimental studies are required.
Empagliflozin therapy, compared to placebo, reduced systolic/diastolic BPs (mean group difference in change from baseline to week 24; −5.9 [95% confidence interval (CI), −10.4 to −1.4] mmHg/−2.9 [95% CI, −6.2 to 0.4] mmHg) and MAP ( −3.8 [95% CI, −7.0 to −0.7] mmHg).
Newer Glucose-Lowering Drugs and Risk of Gout: A Network Meta-Analysis of Randomized Outcomes Trials 2024
Compared with placebo, SGLT2 inhibitors were significantly associated with decreased risk of gout (RR, 0.51; 95% CI, 0.29–0.91) while both GLP-1RAs and DPP-4 inhibitors have no significant effects on gout risk. There were no significant differences between SGLT2 inhibitors and GLP-1RAs (RR, 0.75; 95%CI, 0.31–1.82) and between GLP-1RAs and DPP-4 inhibitors (RR, 0.39; 95%CI, 0.14–1.10).
After reading this entire thread, I am definitely considering starting empaglifozin asap.
Lots of evidence about lots of different benefits. Only fear about weight loss (I’m already very thin).
Is there any evidence of the effects on the gastro system, on the microbiota? (my Achilles’ heel)
I’m not sure that the weight loss effect are universal and that they apply to people already thin (contrary to semaglutide for instance).
Some papers (I probably posted them in this thread) suggest that the effects of SGLT2i are off target via microbiota rebalancing. But that’s just an assumption at this stage.
I wanted some clarification on this topic, so I asked Dr. Oracle and here was his answer. Quite interesting and informative, IMO, so I figured I’d pass it along:
Vascular Calcification in Chronic Kidney Disease vs. Atherosclerosis
Differences in Pathogenesis
Vascular Calcification in Chronic Kidney Disease (CKD)
Occurs primarily in the medial layer of the arterial wall (medial calcification)
Involves transformation of vascular smooth muscle cells (VSMCs) into an osteoblast-like phenotype
Driven by dysregulated mineral metabolism, including elevated calcium, phosphate, and parathyroid hormone levels
Atherosclerotic Calcification
Occurs primarily in the intimal layer of the arterial wall (intimal calcification)
Associated with inflammatory processes and lipid deposition within the atherosclerotic plaque
Driven by traditional cardiovascular risk factors, such as dyslipidemia, hypertension, and diabetes
Clinical Implications
Both forms of vascular calcification are associated with increased cardiovascular morbidity and mortality.
In CKD patients, medial calcification contributes to increased arterial stiffness and left ventricular hypertrophy, leading to cardiovascular complications.
Atherosclerotic calcification is a marker of advanced atherosclerotic disease and increased risk of myocardial infarction and stroke.
Treatment Considerations
CKD-related Vascular Calcification
Strict control of mineral metabolism (calcium, phosphate, and parathyroid hormone levels)
Use of non-calcium-based phosphate binders (e.g., sevelamer, lanthanum carbonate)
Vitamin K supplementation (potential inhibition of vascular calcification)
Atherosclerotic Calcification
Management of traditional cardiovascular risk factors (lipid-lowering, blood pressure control, glycemic control)
Antiplatelet and anticoagulant therapy for secondary prevention
Caveats and Guidelines
There are no specific guidelines for the treatment of vascular calcification in CKD or atherosclerosis.
Treatment strategies are based on managing the underlying disease processes and risk factors.
Early detection and monitoring of vascular calcification through imaging techniques (e.g., computed tomography, ultrasound) are recommended in high-risk populations.
If you’re worried about weight loss, there’s a simple solution. Eat more calories. For most, this is an enjoyable process. I’d love to eat more of my favourite foods without having to worry about adding weight. ![]()
Although your grocery bill may go up and it is possible to overcompensate for the weight loss. ![]()
If caloric restriction is associated with longevity, then too many calories would probably put me in the opposite direction. Anyway, I’ve tried to increase my calories a lot and I still can’t gain weight. I’m celiac, my digestion is poor and nutrient absorption is even worse.
Have you tried gluten free huel?
Oliver Zolman mentions it here:
I Did not know. I’ll take a look, thanks.
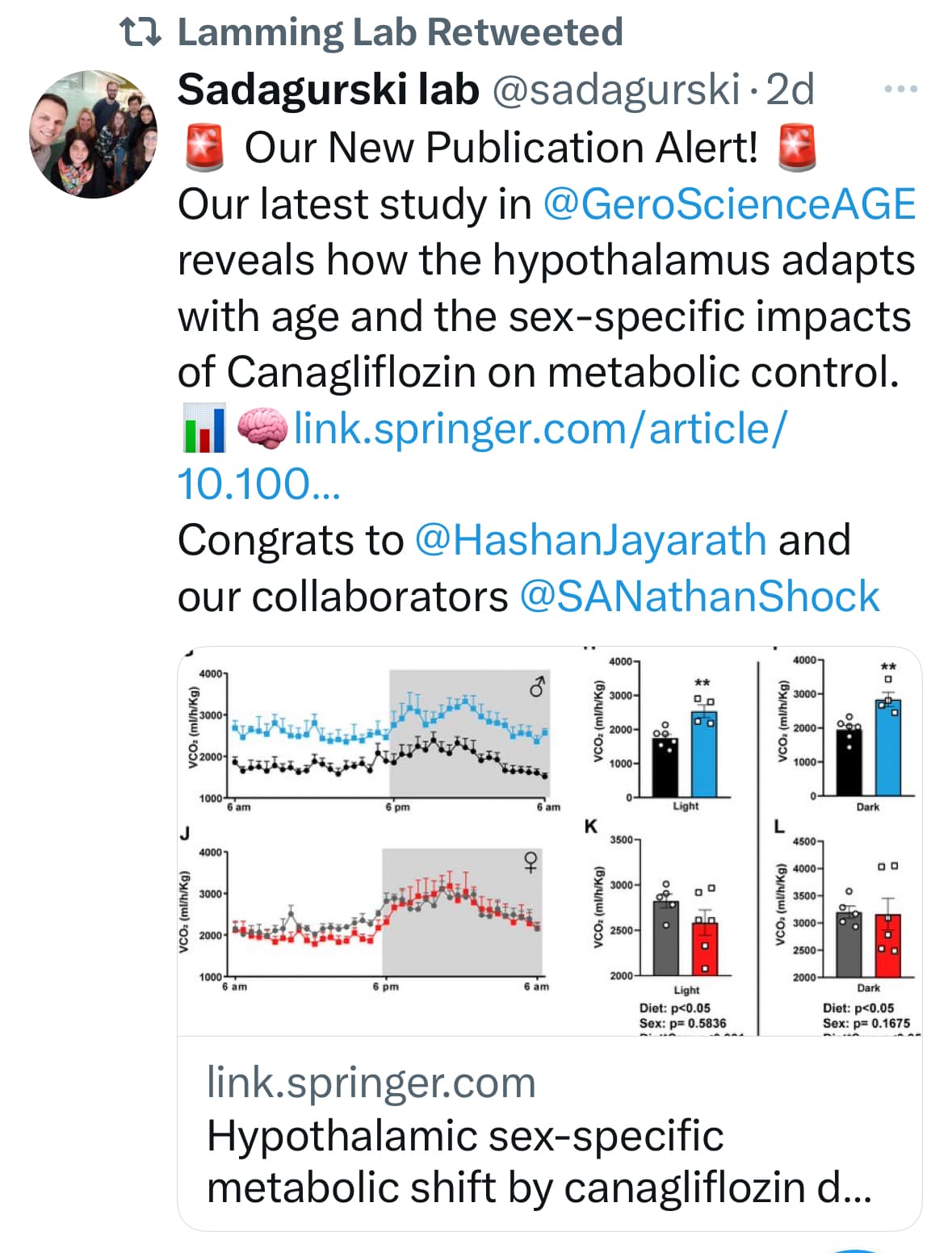
Canagliflozin (Cana), can extend the median survival of genetically heterogeneous UM-HET3 male mice and improve central metabolic control via increases in hypothalamic insulin responsiveness in aged males, as well as reduced age-associated hypothalamic inflammation. We studied the long- and short-term effects of Cana on hypothalamic metabolic control in UM-HET3 mice. Starting the treatment from 7 months of age, we show that 4 weeks of Cana treatment significantly reduced body weight and fat mass in male but not female mice that was associated with enhanced glucose tolerance and insulin sensitivity observed by 12 months. Indirect calorimetry showed that Cana treatment increased energy expenditure in male, but not female mice, at 12 months of age. Long-term Cana treatment increased metabolic rates in both sexes, and markedly increasing formation of both orexigenic and anorexigenic projections to the paraventricular nucleus of the hypothalamus (PVH) mostly in females by 25 months. Hypothalamic RNA-sequencing analysis revealed increased sex-specific genes and signaling pathways related to insulin signaling, glycogen catabolic pathway, neuropeptide signaling, and mitochondrial function upregulated by Cana, with males showing a more pronounced and sustained effect on metabolic pathways at both age groups.
Snake oil!..
Why? Seems quite good to me actually
the stuff you get from it is best sourced by natural, organic food. too expensive also.
If you really want to get proper nutrition, it requires doing what Lustgarten does and it’s a full time job. Nobody really has these answers. Nutrition is the wild wild west. So if there is a market for a complete feed (like we give to confinement animals) and they use it and sell it eventually it could be good. And we can spend our time and energy on other things. So I encourage this attempt and wish them well.
Not at all you can base your nutrition decisions on randomized controlled trials and the totality of evidence from epidemiological studies that control for many confounding factors.