They ship to France, Portugal and Spain apparently. So it might not be an EU wide restriction.
Yes, I’ve used pill splitters for decades. In the case of branded empagliflozin (Jardiance), the pills are elongated and easier to just snap in half rather than bothering with the splitter.
On Metformin vs SGLT2i with respect to serum glucose control I like the idea that SGLT2i’s are more effective at higher glucose levels. So what they do well is prevent serum glucose spikes. I think a lot of the data suggests that controlling the level of these spikes is what is important for longevity (insulin resistance, acarbose data, and SGLT2i all converge around controlling spikes). In the context of the need/desire for muscle gain and the body’s need for glucose at appropriate serum levels it seems SGLT2i’s are more “physiologic” than metformin which basically short circuits the mitochondria. So I would consider using an SGLT2i in place of metformin rather than both together. If you do, you will likely need the higher 25 mg empagliflozin dose to maintain your HbA1C where metformin did without additional changes in diet/lifestyle.
I don’t think they do much for postprandial (i.e. post-meal) glucose spikes, except maybe canagliflozin since it inhibits SGLT1 as well as 2. Someone posted a study, I think way back in this thread, showing the actual data. Since for the SGLT2i drugs all glucose is still fully absorbed, the spike still happens. Acarbose of course severely blunts the spike (but also causes some GI issues since the glucose then gets fermented by the GI flora).
It’s difficult to imagine how sglt2i’s lower HbA1c without lowering postprandial spikes of serum glucose. One of the benefits of SGLT2i is they lower serum glucose without causing hyoglycemia. They do that by preferentially reducing serum glucose levels at the higher end of the range. Including postprandial glucose spikes. The entire blood volume circulates through the kidneys quite quickly, it’s not like you absorb all your glucose at once after a meal and then filter it, it’s being blocked for reabsorption in the kidneys even while levels are increasing after a meal. Its a different mechanism than blocking SGLT1 but the end result is the same. It’s the high glucose spikes that are most damaging to end organs in diabetes.
I don’t agree with the assertion that SGLT2i drugs are at best a waste of money for otherwise-healthy people, but he presents a pretty strong case w/data that they don’t affect postprandial glucose spikes in non-diabetics.
Yes I remember that post. It gets to the point that I was making earlier that low dose and high dose empagliflozin were tested in diabetics and if you want to take these meds as a non-diabetic and hope to affect your serum glucose you are going to need to err on the high end of the dosing range. His/her comments were targeted mainly at the point that cana is different from the other flozins which I agree with for the reasons he states.
Not sure we need to argue about this, but I think that poster’s comments are not correct. I do think his statements are attempting to make the same point I am, that one needs very high plasma glucose levels to see a significant reduction with these meds (ie Diabetes). However, I’m pretty sure a study in normal glycemic individuals would show both a reduction in plasma glucose steady state levels and peak postprandial glucose levels (not saying it will eliminate a postprandial elevation, just limit the height of the peak). Everyone agrees flozin’s lower plasma glucose levels, it doesn’t make any sense that they wouldn’t reduce the peak as well. Plenty of evidence for this with normal glycemic people doing urine dips and showing glucose in their urine, its got to come from somewhere.
Well, he pointed to this study:
Which literally shows no impact on postprandial glucose with dapagliflozin in non-diabetics. “Dapagliflozin had no effect on PPG excursion”, per the abstract. Here’s the chart from the paper:
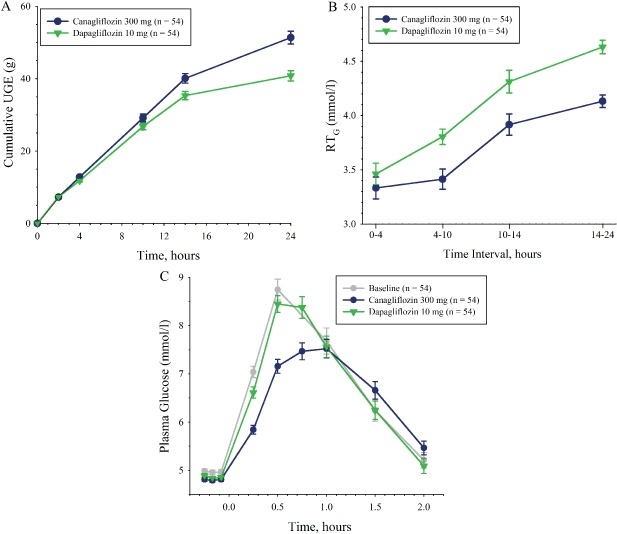
The third one labeled “plasma glucose” is postprandial glucose spike. No significant difference between placebo (gray line) and dapa (green line). Canagliflozin shows a blunting, but it would have to be taken before each meal to get this effect, and only at a dose of greater than 200mg per the other study he posted. Either way, no effect of dapa.
I’m hoping/expecting the benefits of the SGTL2i drugs are independent of postprandial glucose or glucose altogether. After all, if the only thing these drugs are doing is causing us non-diabetics to excrete an extra 50g of glucose in our urine per day and there are no other beneficial tissue-specific SGLT2i effects, then we’d get all the benefits, NO potential side effects AND save a lot of money by just eating 50g less of carbs per day.
How silly are we all going to feel if it just comes down to that? ![]()
I can eat almost no carbs per day, I do it all the time. Still I end up with pretty high (~90 or 105) fasting glucose. So would Cana help burn that up all day long and lower my hba1c by a bit, or will my liver compensate and keep the sugar high?
FYI: in this small trial in people with MCI but without T2D after 12 weeks they observed a small reduction in Hb A1C (-0.18) and what I think is a more significant reduction in “2-hr Glucose Area Under the Curve (- 2109.0 mg min/dL, p=0.03)”.
There are many very large trials of SGLT2 in non-diabetic people (for CKD and HF). For instance, in DAPA-CKD, “of 4,304 participants, 738 had normoglycemia, 660 had prediabetes, and 2,906 had type 2 diabetes.” They found that (see: Efficacy and Safety of Dapagliflozin by Baseline Glycemic Status: A Prespecified Analysis From the DAPA-CKD Trial 2021):
The effect of dapagliflozin on the primary outcome was consistent (P for interaction = 0.19) in normoglycemia (hazard ratio [HR] 0.62 [95% CI 0.39, 1.01]), prediabetes (HR 0.37 [0.21, 0.66]), and type 2 diabetes (HR 0.64 [0.52, 0.79]).
Our findings from a dedicated kidney outcome trial substantiate the findings from the Canagliflozin and Renal Events in Diabetes With Established Nephropathy Clinical Evaluation (CREDENCE) study, suggesting that the kidney benefits seen with SGLT2 inhibition appear to be independent of their glucose-lowering effects, and extend these results further to those with prediabetes and normoglycemia at baseline.
Few studies have investigated SGLT2 inhibition in prediabetes. During a 13-week randomized comparison between dapagliflozin, metformin, exercise, or control intervention, Færch et al. found that dapagliflozin treatment led to improved glycemic variability, with minor reductions in HbA1c (0.1% or 1.3 mmol/mol) and fasting plasma glucose (0.1 mmol/L or 1.8 mg/dL).
In participants with normoglycemia or prediabetes, dapagliflozin reduced the risk of kidney outcomes without improving glycemic control. These data are in keeping with an analysis of the CANagliflozin cardioVascular Assessment Study (CANVAS) trial, where markers of glycemia did not explain the effect of canagliflozin on kidney outcomes. Instead, albuminuria, hemoglobin, and hematocrit were identified as important mediators, pointing to a potential reduction in fluid overload. The recognized effect of SGLT2 inhibitors on hemoglobin and hematocrit may reflect improvement in renal hypoxia and restoration in the hypoxia-inducible factor 1α/2α balance, stimulating erythropoiesis and reducing inflammation. Glucose-independent effects may include osmotic diuretic and natriuretic effects as observed in individuals with type 2 diabetes and CKD.
(since then, a recent paper showed that the benefits were probably not due to osmotic diuretic effects, so it’s still a mystery ![]() )
)
Here’s the paper on variability: The effects of dapagliflozin, metformin or exercise on glycaemic variability in overweight or obese individuals with prediabetes (the PRE-D Trial): a multi-arm, randomised, controlled trial 2020
One hundred and twenty participants with BMI ≥25 kg/m2, 30–70 years of age, and prediabetes (HbA1c 39–47 mmol/mol [5.7–6.4%]) were randomised 1:1:1:1 to dapagliflozin (10 mg once daily), metformin (1700 mg daily), interval-based exercise (5 days/week, 30 min/session) or control (habitual lifestyle). Participants were examined at baseline and at 6, 13 and 26 weeks after randomisation. The primary outcome was the 13 week change in glycaemic variability (calculated as mean amplitude of glycaemic excursions [MAGE]) determined using a continuous glucose monitoring system (pre-specified minimal clinically important difference in MAGE ∼30%).
One hundred and twelve participants attended the examination at 13 weeks and 111 attended the follow-up visit at 26 weeks. Compared with the control group, there was a small decrease in MAGE in the dapagliflozin group (17.1% [95% CI 0.7, 30.8], p = 0.042) and a small, non-significant, reduction in the exercise group (15.3% [95% CI −1.2, 29.1], p = 0.067), whereas MAGE was unchanged in the metformin group (0.1% [95% CI −16.1, 19.4], p = 0.991)). Compared with the metformin group, MAGE was 17.2% (95% CI 0.8, 30.9; p = 0.041) lower in the dapagliflozin group and 15.4% (95% CI −1.1, 29.1; p = 0.065) lower in the exercise group after 13 weeks, with no difference between exercise and dapagliflozin (2.2% [95% CI −14.8, 22.5], p = 0.815).
So dapagliflozin improves the glycemic variability of prediabetic overweight people as much as daily interval training. What about normoglycemic non-overweight people?
This study was done after 4 days. My guess (based on my own experience + the above papers) is that the effects of SGLT2i are more systemic and take a few weeks or months to kick in.
Thanks! Is there a link to this study in your post? Or is that part of one of the other studies you mentioned?
Regarding the glycemic variability study vs exercise vs metformin, that is interesting although the authors note the effect is “small” and “clinical significance unknown”. I’m eager to get more data on any non-glucose-related effects of these meds.
Yes, I replied to the original post that includes the poster: Canagliflozin - Another Top Anti-aging Drug - #750 by adssx
The vast majority of their positive effects are glucose-independent. That’s why SGLT2is are approved in CKD and HF, contrary to other antidiabetic drugs (and they might be extended to NAFLD and HCM). And that’s also why they protect more from AD and dementia than other anti-diabetic drugs. See here for some overviews: Acarbose - Details On Another Top Anti-Aging Drug - #448 by adssx
Looking at those diagrams, though – don’t they all start with glycosuria? One points out increased sodium excretion as well. All the other beneficial effects appear to be downstream, don’t they? If this is the case, couldn’t we get these same downstream benefits by simply eating less sodium and sugar?
(Note I don’t want the above to be true. I take empagliflozin and I want to believe this med is useful!)
- One of the diagrams doesn’t start with glycosuria

- The diagrams are, of course, simplifications. And we cannot draw what we don’t know: we know that the benefits are largely glucose-independent (as other antidiabetic drugs don’t do as well and as the benefits are independent from baseline Hb A1c and Hb A1c reduction). The articles say:
- “These benefits have been demonstrated in trials of SGLT2is, and appear, to some degree, to be independent of glycemia and substantial weight loss.”
- “Otherwise stated, these agents have direct, glycosuria-independent, effects that decrease cellular stress and enhance cell survival.”
- Risk of dementia divided by 2 compared to other anti-diabetic drugs (DPP-4i): Canagliflozin - Another Top Anti-aging Drug - #723 by adssx
- ACM divided by 2 vs metformin: Canagliflozin - Another Top Anti-aging Drug - #705 by adssx (see also the paper explaining their potential off-target mechanisms “including the inhibition of gut microbiome–mediated uremic toxin formation”)
So no, just reducing one’s sugar intake is not equivalent to taking SGLT2.
Yes that’s true, but it’s still possible those could be downstream effects. What I’m looking for is a mechanistic explanation that ties SGLT2 inhibition to all of these effects, other than glycosuria/natriuria. We don’t have that yet, do we?
Considering the beneficial effects the flozins have on kidney function, maybe the longevity effects are related to that?
No, we don’t have one. Mechanistic explanations are useless scientistic hubris. We don’t even know how paracetamol works.
Oh c’mon now. We have plenty of nice mechanistic data for all kinds of drugs. Look at rapamycin and mTOR! By knowing how things work, it opens up possibilities for other targets in the pathway(s) which may be even safer and/or more effective.
Yes but, according to Brian Kennedy, 10–20% of current drugs have the wrong target: https://www.youtube.com/watch?v=RQeylLfMpoo
And I think that this doesn’t include drugs with additional unknown targets. Mechanistic theories are interesting, but in some situations, such as for SGLT2i, they’re useless.
That’s why Eric Schmidt funded EveBio to map all FDA-approved drugs and targets. They’ve told me they’ve already found some crazy results. The data will be published in open data later this year.
You’d still need clinical trials for those targets in the same pathways either way for it to be comparable. If you believe sodium or sugar restriction would have the same benefit, you can look up if such clinical trials exist.