That’s how I did the maths, assuming that “No. reports of events other than MS” is somewhat proportional to the use of the drug. In any case, we need more data on this. There’s an ongoing trial of metformin for MS: https://www.mssociety.org.uk/research/explore-our-research/emerging-research-and-treatments/explore-treatments-in-trials/metformin Two weeks ago I met with the charity behind this trial and suggested to test next GLP-1RAs and SGLT2is but they didn’t seem super interested (not sure they were aware of what SGLT2i were…). I’ve just sent them the paper, wait and see. ![]()
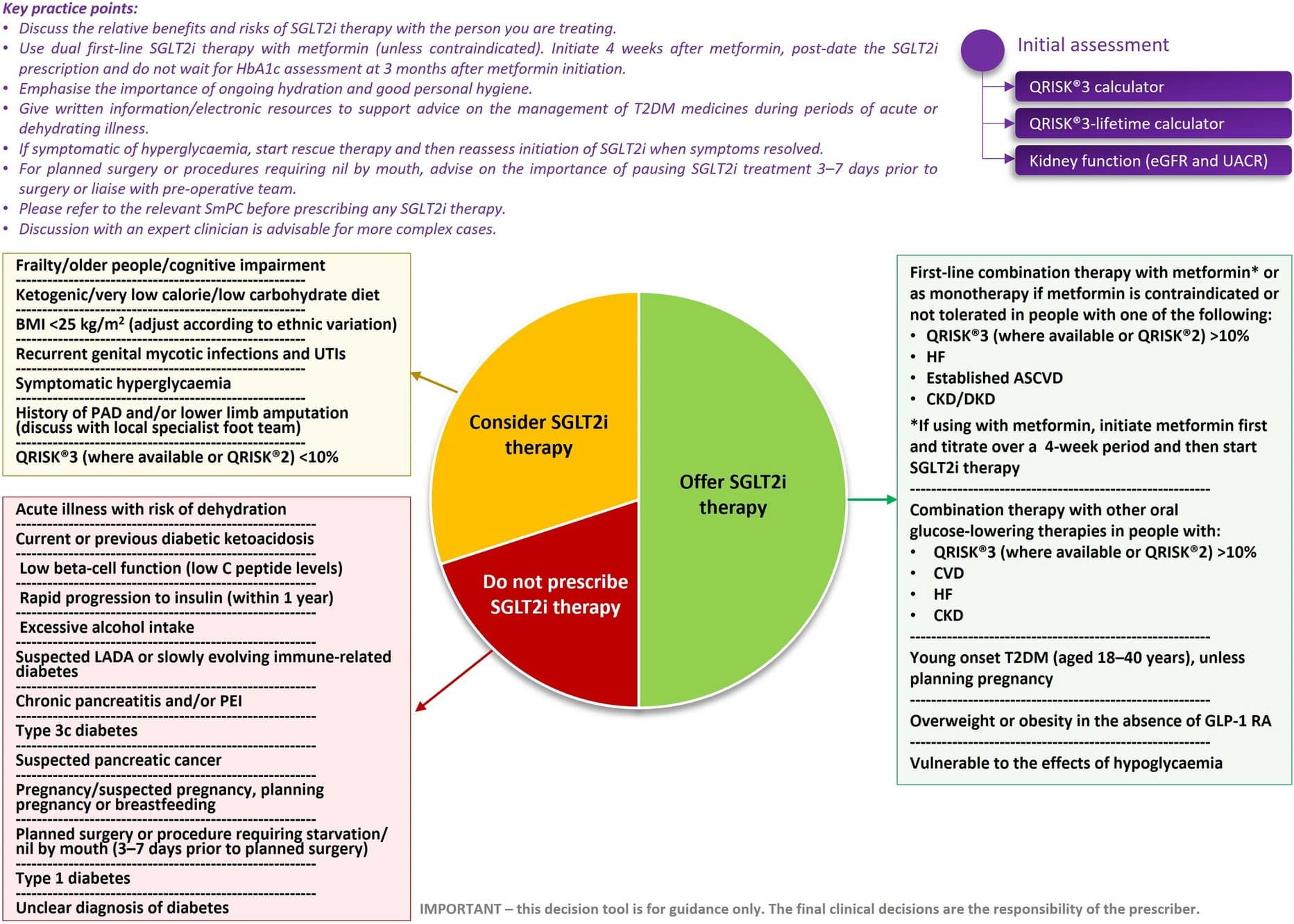
Considering the wealth of data supporting these medicines, the Improving Diabetes Steering Committee (IDSC) expects SGLT2i therapies to take a more prominent role in future guidelines, potentially as a key component of standard care for newly diagnosed individuals with T2DM.
The expansive evidence-base indicates that the proven advantages of SGLT2is in slowing or preventing the onset of serious CVRM complications and maintaining durable health outcomes should outweigh (or place into context) manageable issues (e.g. mycotic genital infections) and perceived potential risk of rare adverse events that may have previously delayed or deterred prescribing of these medicines for the right individuals.
Putting the evidence in to practice, the IDSC supports the implementation of a rapid sequential approach to T2DM management comprising early combination therapy with metformin and an SGLT2i agent for most people with T2DM, rather than gradual stepwise intensification of treatment over an extended period. Using this method, metformin should be initiated and titrated to an appropriate dose during the first month, with the SGLT2i agent added (unless contraindicated) after 4 weeks (supported by a telephone appointment, where possible) or by a review after 12 weeks (at latest). For high-risk individuals (high CV risk, CVD or kidney disease), an SGLT2i should be started at diagnosis, with or without other diabetes therapies, in line with ADA/EASD and KDIGO guidelines
Methods: This was a collaborative trial-level meta-analysis from the SGLT2i meta-analysis cardio-renal trialists consortium, which includes all phase 3, placebo-controlled, outcomes trials of SGLT2i across three patient populations (diabetes at high risk for atherosclerotic cardiovascular disease [ASCVD], heart failure [HF], or chronic kidney disease [CKD]). The outcomes of interest were MACE (composite of CV death, myocardial infarction [MI], or stroke), individual components of MACE (inclusive of fatal and non-fatal events), all-cause mortality, and death subtypes. Effect estimates for SGLT2i vs. placebo were meta-analyzed across trials and examined across key subgroups (established ASCVD, prior MI, diabetes, prior HF, albuminuria, CKD stages and risk groups).
Results: A total of 78,607 patients across 11 trials were included: 42,568 (54.2%), 20,725 (26.4%), and 15,314 (19.5%) were included from trials of patients with diabetes at high risk for ASCVD, HF, or CKD, respectively. SGLT2i reduced the rate of MACE by 9% (HR 0.91 [95% CI 0.87-0.96], p<0.0001) with a consistent effect across all three patient populations (I 2=0%) and across all key subgroups. This effect was primarily driven by a reduction in CV death (HR 0.86 [0.81-0.92], p<0.0001), with no significant effect for MI in the overall population (HR 0.95 [0.87-1.04], p=0.29), and no effect on stroke (HR 0.99 [0.91-1.07], p=0.77). The benefit for CV death was driven primarily by reductions in HF death and sudden cardiac death (HR 0.68 [0.46-1.02] and HR 0.86 [0.78-0.95], respectively) and was generally consistent across subgroups, with the possible exception of being more apparent in those with albuminuria (Pint=0.02).
I think this reinforces the fact that arteriosclerosis is made noticeably worse by diabetes and high blood sugar levels.
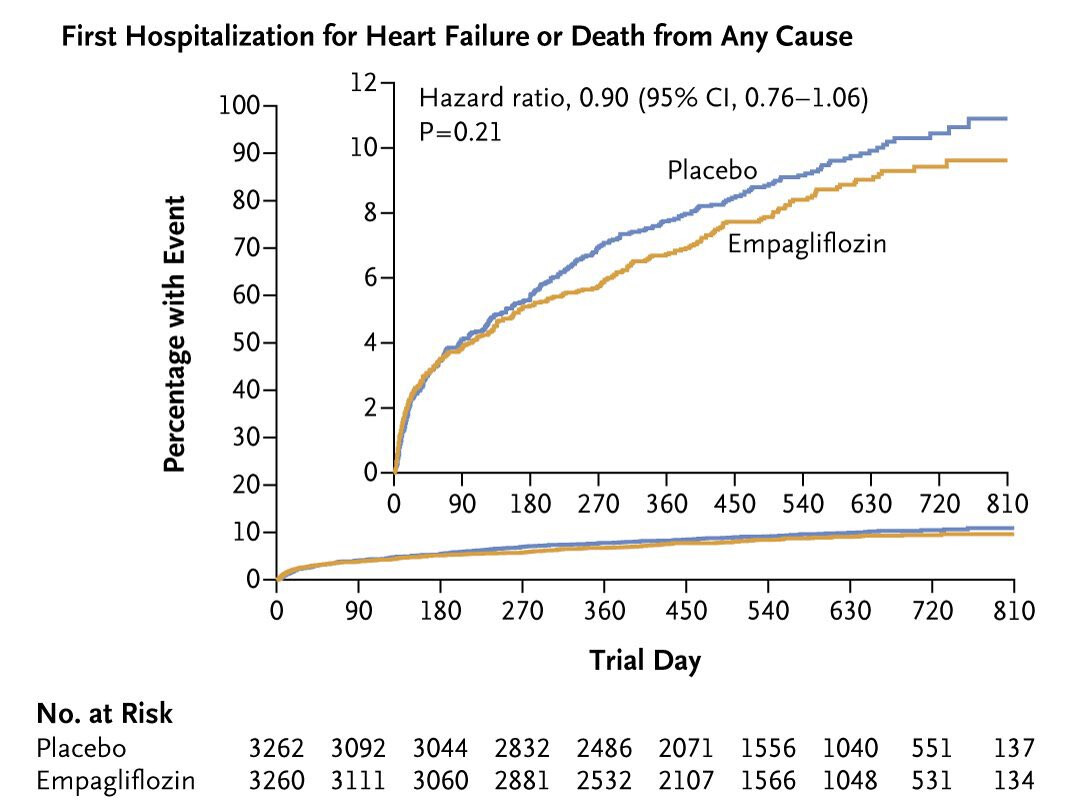
Three articles published on the same day in three different journals by the same authors about the same EMPACT-MI trial (6,522 patients hospitalized for acute myocardial infarction at risk for heart failure), funded by Boehringer Ingelheim and Eli Lilly:
- Effect of Empagliflozin on Heart Failure Outcomes After Acute Myocardial Infarction: Insights from the EMPACT-MI Trial: “In patients after acute myocardial infarction with left ventricular dysfunction or congestion, empagliflozin reduced the risk of heart failure.” (RR 0.67 [95% CI 0.51, 0.89], P=0.006 for total heart failure hospitalizations)
- Left Ventricular Function, Congestion, and Effect of Empagliflozin on Heart Failure Risk After Myocardial Infarction: “Empagliflozin reduced first and total HF hospitalizations across the range of LVEF with and without congestion.”
-
Empagliflozin after Acute Myocardial Infarction: “Among patients at increased risk for heart failure after acute myocardial infarction, treatment with empagliflozin did not lead to a significantly lower risk of a first hospitalization for heart failure or death from any cause than placebo.” but “a first hospitalization for heart failure occurred in 118 patients (3.6%) in the empagliflozin group and in 153 patients (4.7%) in the placebo group (hazard ratio, 0.77; 95% CI, 0.60 to 0.98), and death from any cause occurred in 169 (5.2%) and 178 (5.5%), respectively”
- Do they have to conclude like this because it was the primary end point?! Is it the reason why they published 2 other papers to “mask” that one?
The trend for empagliflozin looks good to me (gap between placebo and empagliflozin seems to be increasing and upper bound of the 95% CI is 1.06):
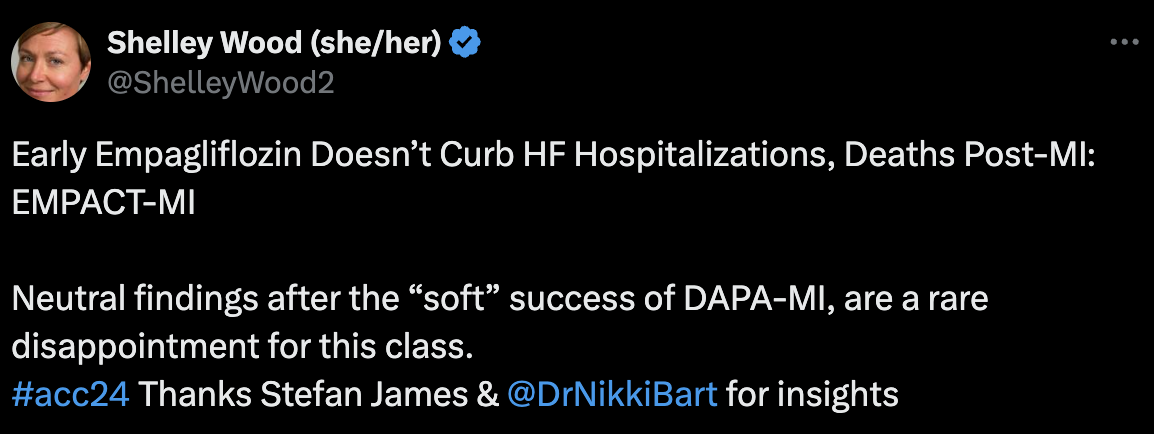
Last year, AstraZeneca did a similar trial (DAPA-MI): Canagliflozin - Another Top Anti-aging Drug - #510 by adssx
If I understand correctly, the two trials differed in their design: Sodium Glucose Co-Transporter 2 Inhibition Following Acute Myocardial Infarction: The DAPA-MI and EMPACT-MI Trials
DAPA-MI was commented back then as a win:
So… is dapagliflozin better than empagliflozin post-MI? Maybe. But does it matter for people here who want to prevent MI and not just to manage the damage already caused: I don’t think so.
Insulin-like growth factor binding protein-7 concentrations in chronic heart failure: Results from the EMPEROR programme 2024 (@Neo)
Across the entire left ventricular EF spectrum in the EMPEROR Programme, concentrations of the senescence-associated biomarker IGFBP7 were associated with higher risk clinical status and predicted adverse cardio-renal outcomes even in models adjusted for conventional biomarkers. Empagliflozin did not significantly affect IGFBP7 levels over time.
Water Conservation Overrides Osmotic Diuresis During SGLT2 Inhibition in Patients With Heart Failure 2024
These findings suggest that SGLT2i may not improve cardiac health status by osmotic diuretic decongestion. An alternative “nutrient deprivation signaling/autophagy hypothesis” assigns the beneficial effects of SGLT2i to reprogramming of mitochondrial function. Similar switches in mitochondrial fuel utilization occur in “aestivation,” an evolutionary conserved survival strategy in response to combined energy and water deficit. The observed ≈150 kcal/d loss of glucose fuel into the urine (Figure 3D) not only requires adaptive energy conservation to prevent an energy deficit but also triggers physiological water conservation to counteract the osmotic diuretic effect of glucosuria and prevent dehydration (Figure 4C). As an extension to the “nutrient deprivation signaling/autophagy hypothesis,” we suggest that SGLT2 inhibition may result in a biomimicry of aestivation metabolism and thereby improve health span.
The interplay between sodium/glucose cotransporter type 2 and mitochondrial ionic environment 2024
SGLT2 may influence mitochondrial dynamics by metabolic/second messenger pathways or by ionic mechanisms.
SGLT2 may mediate ionic mitochondrial environment through a change in intracellular Na+.
Comparison of incident hypertension between SGLT2 inhibitors vs. DPP4 inhibitors 2024
SGLT2i administration was associated with a reduced risk of hypertension (HR 0.91, 95% CI: 0.84–0.97). The advantage of SGLT2i use over DPP4i use for incident hypertension was generally consistent in several sensitivity analyses, and subgroup analyses showed that SGLT2i use was significantly associated with a lower risk of hypertension in men, patients with baseline HbA1c of <7.5%, and baseline systolic blood pressure ≥127 mmHg. Our investigation using nationwide real-world data demonstrated the potential advantage of SGLT2i over DPP4i in reducing the development of hypertension in individuals with diabetes.
The incidence of dementia was 2.7% (4,202/155,844) in the SGLT2i group and 8.7% (26,366/304,268) in the control group (RR 0.50; CI 0.37–0.66; P<0.001).
SGLT2 inhibitors are associated with a significant reduction in the risk of dementia in patients with T2DM. These findings suggest that SGLT2 receptor may be a promising therapeutic target for the prevention of dementia in this population.
@DrFraser, this is massive (and it’s just one among many papers finding similar RRs for SGLT2). I don’t have the full paper, would be great to see if they identified differences between the various SGLTi.
Compared with 1928 patients receiving metformin‐based regimens, 964 patients receiving SGLT2 inhibitor‐based regimens had similar all‐cause mortality (hazard ratio [HR], 0.75 [95% CI, 0.51–1.12]), cardiovascular death (HR, 0.69 [95% CI, 0.25–1.89]), hospitalization for heart failure (HR, 1.06 [95% CI, 0.59–1.92]), stroke (HR, 0.78 [95% CI, 0.48–1.27]), and progression to end‐stage renal disease (HR, 0.88 [95% CI, 0.32–2.39]). However, SGLT2 inhibitors were associated with a lower risk of all‐cause mortality (HR, 0.47 [95% CI, 0.23–0.99]; P for interaction=0.008) and progression to end‐stage renal disease (HR, 0.22 [95% CI, 0.06–0.82]; P for interaction=0.04) in patients under the age of 65.
In comparison to metformin‐based regimens, SGLT2 inhibitor‐based regimens showed a similar risk of all‐cause mortality and adverse cardiorenal events. SGLT2 inhibitors might be considered as first‐line therapy in select low‐risk patients, for example, younger patients with diabetes.
WOW again, the ACM RR under 65 is crazy.
Unexpected metabolic effects of sodium-glucose cotransporter 2 inhibitors 2024
The authors provide insight into 2 novel overarching mechanisms for cardiovascular protection by SGLT2i. First, SGLT2i alter the excretion of many metabolites with cardiovascular relevance, such as the purine metabolite uric acid. Second, SGLT2i modify the microbiome in wild-type mice on the proteome level, mostly in a beneficial direction, as evidenced by a reduction in the microbiotic formation of circulating uremic toxins. This effect appears to occur, at least in part, via a direct, off-target, effect of drug on anaerobic fermentation in the stool.
Taken together, SGLT2 inhibitors establish a favorable metabolic environment and functional state in the early proximal tubule, offering potential kidney and heart protection. Mechanisms are in part off-target, including the inhibition of gut microbiome–mediated uremic toxin formation. These effects have the potential to positively influence blood pressure, volume retention, and the uremic syndrome, ultimately benefiting cardiovascular health.
@Neo this is super interesting if the longevity effects are actually off-target (although we still have one MR paper for SGLT1i being pro-longevity).
It’s also very interesting that several aspects are seen more in “healthy” wild type than the diseases diabetic mice.
I which there was more data on SGLT-i in healthy mice and healthy humans.
Proteomics analysis quantified a total of 9501 proteins (8421 genes) and 10,744 phosphorylation sites in the kidney, liver, heart, muscle, and white adipose tissue. SGLT2i treatment led to significant protein changes. Most of these were observed in the kidney cortex, with much stronger effects in wild-type than diabetic mice. In fact, SGLT2i-induced perturbations in several omics analyses were greater in nondiabetic animals, something the authors attribute to the greater effect of SGLT2i on glycosuria, calorie loss, and proximal tubular glucose content in nondiabetic animals, and which they note has been reported by others. < @adssx do you know which others?
Moreover, only wild-type mice reacted to SGLT2i with downregulation of kidney proteins, mostly transmembrane transporters localized to the apical or basolateral membrane, or proteins involved in mRNA splicing. Using interactome analysis of SGLT2, they found that this transporter interacted with sodium- and hydrogen transporter–regulating proteins and also with several metabolite transporters, both in the mouse and in the human kidney. SGLT2 inhibition changed the global phosphoproteome landscape, including metabolically regulated proteins, primarily in the mouse kidney. Closer analysis of amino acid sequences surrounding phosphorylation sites revealed distinct alterations in wild-type mice but also in diabetic mice. Substantial proteome and phosphoproteome changes also occurred in the heart, liver, adipose tissue, and other organs.
@adssx have you looked anything at the main actual paper this discussion is about?
I wish they could do this analysis where they compare how the extent of SGLT1 vs SGLT2 inhibition of SGLT-i drugs impacts above (since we known SGLT1 works more via the gut).
This is till my biggest question mark about SGLT-i - how come we don’t see more MR studies connected to longevity and mortality? Are the genetic instruments for SGLT2 (and 1) not good or difficult and therefore people don’t spend time doing these type of analyses? Or are people doing them, not seeing results and then not published no-result papers?
I didn’t read the commented paper (I should!) and I missed this excellent point when skimming through the commentary. Thanks.
My guess is that they don’t have enough data. SGLT2i are so new (~2013, vs 2004 for GLP-1RAs) and it’s only now that they’re becoming mainstream (see the recent papers above arguing for their generalization as first-line treatments in T2D). There’s so much “hype” around SGLT2 that even negative results would be worth publishing for a researcher I think, it would also from a theoretical point of view confirm that off target pathways are part of the benefits.
I don’t have access to the full article - but mortality here seemed positively impacted.
https://dom-pubs.pericles-prod.literatumonline.com/doi/epdf/10.1111/dom.14286
It is also an issue where even the studies in the article above simply had to be 12 months or more - and naturally the patients have a medical condition necessitating an SGLT2-i.
I’m not sure we’ll see a study any time soon of individuals in their 40’s-80’s just taking these to reduce their risk of death and following them for a decade. We are in the same conundrum with rapamycin - we think we have solid reason to believe benefit - which could be substantial, but we don’t have the definitive study, nor is it likely forthcoming quickly … all while the clock is ticking.
Thx.
21 trials were selected, enrolling 39 593 and 30 771 patients in SGLT2 inhibitor and comparator arms, respectively, with a median duration of 104 weeks, and reporting 2474 and 2298 deaths for SGLT2 inhibitors and comparators, respectively. No relevant heterogeneity was found (I2 = 17%). Treatment with SGLT2 inhibitors was associated with a significant reduction in all-cause mortality (MH-OR [95% CI] 0.86 [0.81, 0.91] P < .00001). Meta-regression analyses found a significant direct association of treatment effect only with the proportion of Asian subjects enrolled, and an inverse correlation with the proportion of Caucasian patients. In conclusion, SGLT2 inhibitors reduce all-cause mortality in randomized controlled trials.
Interesting with the ethic genetic background having a meaningful effect in the meta analysis
Totally. Hopefully Mendelian Randomization studies can help fill some of the gaps with that.
I think (hope?) we’ll get that kind of data in a few years. All healthcare systems (except in the US of course ![]() ) are building (or have already built) massive data collection systems to allow for these studies. A friend of mine has access to the EMR of 60m French people, hopefully with such massive datasets you can detect even small signals of recent drugs like SGLT2. Combined with MR studies
) are building (or have already built) massive data collection systems to allow for these studies. A friend of mine has access to the EMR of 60m French people, hopefully with such massive datasets you can detect even small signals of recent drugs like SGLT2. Combined with MR studies
The EPIC EMR has this ability - actually worldwide. To my knowledge - the data is available depersonalized for researchers. So this should be an option within the U.S., but also through the international sites that use this EMR. Most of the major academic institution in the U.S. use EPIC.
The issue in the US is that you have different private and public insurers and people might switch over their lifetime from one to the other (changing job, moving to another state, change of socioeconomic conditions) so it’s harder to follow someone from the cradle to the grave. That’s why most US researchers work and publish papers on European databases. In Europe (and in most of the world actually) you have one centralized EMR with everything. Now they’re merging national EMRs into a European Data Healthy Hub so you’ll have half a billion people in one database with test results, prescriptions and diagnoses.
Indeed - fragmentation in care is a huge issue in the U.S. This also relates to why insurers often times don’t cover really sensible treatments that decrease long term health risks. The presumption is the patient is going to not be in their health plan 2 years from now … so why fund something that might not make a difference for 10 years?
Yes, in the fantastic Acquired podcast on Ozempic, they say:
The average American in the private sector holds a job for 3.7 years That means that on average, insurance companies are going to churn you every 3.7 years or sooner if your company changes the insurance plan. Their incentive is to cover you only in two categories of things. (1) Things that pay themselves back in less than 3.7 years. (2) Things that have such an overwhelming demand from employees that their employers think that they absolutely have to cover them to stay competitive.
You have the same issue with all “longevity” drugs.
Still, you face a similar problem in socialized healthcare systems: people don’t churn, but decision-makers have term limits: why would a politician cover a treatment today and increase costs only for long-term benefits that their successors (and often political opponents) will reap? Unless the treatment is highly popular and can bring votes at the next election, or if the decision to re-imburse or not each treatment is made by a highly independent board with long-term goals (which is in theory the case but in practice…).